Invest in ME Research International ME Conference 2018
Thirteen years of Commitment to Biomedical Research into ME

Click on sections below
13th Invest in ME Research International ME Conference
CONFERENCE REPORT
by Invest in ME Research
The 13th Invest in ME Research International ME Conference on 1st June 2018 in Westminster, London, followed the
2 day International
Biomedical Research into ME colloquium where the major institutes and researchers from around the world
gathered to discuss their work.
At the conference there was a full day of presentations by a wide range of International speakers on a variety of associated topics.
Dr Ian Gibson
Welcome to IIMEC13
Dr Ian Gibson opened the meeting referring to the previous days’ events.
He especially liked the
Thinking the Future early career event which had been organised by
Invest in ME Research three days ealier

during ME Conference Week,
where young researchers were able to present and network in a friendly and supportive atmosphere.
He also mentioned that the science being presented at the
BRMEC8 Colloquium was getting
better each year and it would not be long
before someone comes up with a eureka moment.
He mentioned how pleased he was that each presentation took patients into account and it was not just a case of showcasing one’s science.
Patients were at the heart of each presentation.
Dr. Elizabeth R. Unger
Research Update from CDC
Dr Elizabeth R. Unger, CDC talked about new Initiatives and gave an update on CDC activities.
The CDC is a huge organisation and it tracks
public health. The aim is to add ME/CFS into the CDC’s mainstream programme.
One of the tracking systems the CDC use is the Behavioural Risk Factor Surveillance (BRFSS) that was set up in 1984 involving 15 states.
The surveillance has now been extended to all 50 states, district of Columbia and three territories.
They interview more than 400,000 adults each year.
Data is collected on health related behaviours, chronic health conditions and use of preventive services.
This data is available at state level which makes it
useful for local information/planning and will help in estimating prevalence numbers and disease
burden that are currently lacking in ME/CFS in a sustainable way.
ME/CFS was first presented to be adopted to this surveillance system in 2013 but was not approved then even though five states added it to their
programmes.
A new presentation for the case was made in 2018 and the proposal was approved so ME/CFS has now been accepted
as a new optional module for 2019.
The benefit of this surveillance tool is that ME/CFS can be tracked to many variables such as quality of life, physical activity, comorbidities etc.
The reason for ME/CFS being accepted to the programme now is probably due to increased persistence, advocacy and the CDC presenting at public conferences.
They would also like to add active surveillance in schools and ME/CFS diagnoses integrated into health systems such as Vaccine Safety Datalink (VSD)
project.
CDC also recognises the importance of healthcare education.
The webpages have been updated to reflect the IOM report and there is going to be an educational video provided by Medscape on how to diagnose
ME/CFS featuring four doctors (Lucinda Bateman, Natalie Azar, Nancy Klimas and Jose Montoya).
A roundtable involving stakeholders is being planned for the end of 2018.
An update of the CDC multisite study that involves seven clinicians/clinics was set out to test out the comparability of cases diagnosed by experienced
ME experts.
Data has been collected to standardise methods such as physical testing.
CDC has joined efforts with NIH in the common data elements project that will help in standardising research.
Dr Vicky Whittemore NIH
NIH Common Data Elements
 Dr Vicky Whittemore NIH gave an update on NIH activities and the NIH/CDC Common Data Elements.
Dr Vicky Whittemore NIH gave an update on NIH activities and the NIH/CDC Common Data Elements.
Dr Whittemore started by referring to IiMER opening comments that one can talk about doing things but it is not until “the rubber hits the road” and you take action that is important. Funding from the NIH for ME/CFS since the fiscal year of 2016 to 2017 has doubled but it is clearly not enough. The NIH is encouraging more funding applications submitted to them. They have 27 institutes that fund research and from 2016 to 2017 the number of institutions interested in funding ME/CFS research has increased from 8 to 12.
Dr Whittemore then mentioned the recent funding given to three research centres and one data centre.
- Cornell University (Maureen Hanson) will concentrate on the biological mechanisms and looking at baseline measurements before and after exercise challenges.
- Columbia University (Ian Lipkin) will utilise their existing samples to look for microbial agents and triggers playing a role in initiating ME/CFS. They will also do a comprehensive genomic analysis to identify potential metabolites that might be present.
- Jackson laboratories (Derya Ununmatz) will take a detailed look at how the immune system, the microbiome and metabolism interact in ME/CFS.
These centres are also required to set aside money for a collaborative project that they are in the process of putting in place. The NIH is also collaborating with the Canadian Research Council that has set aside money for applications for a Canadian ME/CFS research centre. At the NIH each institute has an advisory council that is made up of clinicians, researchers and patients and patient advocates and Dr Whittemore announced the working group of NINDS Advisory Council that helps progress ME/CFS research. The group is chaired by Steven Roberds, CSO of the Tuberous Sclerosis Alliance and NINDS Advisory Council member and additional members will be invited by NINDS director Walter Koroshetz. The working group will then give guidance to the National Advisory Neurological Disorders and Stroke Council (NANDS), Dr Koroshetz and the trans NIH working group.
Dr Whittemore also announced the date for a NIH ME/CFS conference to be held in Bethesda on the 3-4 April 2019 and as she was impressed by the young investigator workshop organised by IiMER then she will work with IiMER and the Thinking the Future group to continue and repeat this in the US. Dr Whittemore then went on to describe the Common Data Elements (CDE) project that she thought had started as long as ten years ago. The aim was to harmonise information/to create common language so that researchers will be reporting their data in the same way all over the world. This would help make data comparable across studies. This is a dynamic and evolving process as more is known about the disease. The objectives of the CDE project is to identify CDEs used in clinical research, present data elements in standard form, identify common definitions, standardise CRFs (Common Report Forms) and to provide information to researchers for clinical data collection and sharing. The work started in December 2016 and finished in February 2018. The project was divided into 11 subgroups. All the groups held conference calls and discussed matters. Documents were produced and reviewed first internally before being released for public comment and now they have been published on the NIH website. There will be ongoing revision and review so it is a dynamic process. The members of the sub groups are now preparing a publication about the process of this project.
Dr Whittemore described the subdomains that included everything from the basics such as fatigue to biomarkers and explained how the CDE terminology/classification includes general core, disease core, supplemental (highly recommended), supplemental and exploratory (such as biomarkers) information. The working group involved participants from all over the world and it was the first time that a CDE NIH working group had included patients and patient advocates from the beginning of the process and not just allowed them to comment on the finished product.
Dr Whittemore stated that it was a very positive experience. There was a question from the audience whether the UK NICE spoke to NIH and the answer was yes and Dr Whittemore hoped that NICE would adopt the CDEs. Dr Unger was asked why the CDC chose to do only a one day CPET test and Dr Unger replied that this was based on the advice of the clinicians involved. The patients would find a two day test too difficult to perform and the purpose of the CDC study was not to diagnose patients but to follow cognitive and other symptoms after a major exercise challenge. Dr Unger said the CDC discussed this a lot and they also consulted the Workwell Foundation on this. The Workwell Foundation preferred the two day test but understood reasons for the one day test. The CDC also enlisted the help of Dane Cook and felt the data (not yet unblinded) will be valid for the purpose.
Dr Avindra Nath NIH
Challenges in study design and identification of patients with post-infectious ME
Dr Avindra Nath NIH talked about Challenges in Study design and Identification of patients with Post-Infectious ME/CFS. Dr Nath started by commenting on the superb two day colloquium that took place ahead of the conference. He thought the scientific data emerging is unprecedented. Dr Nath wanted to make the presentation more of a dialogue than presentation as he has learned so much from discussions with the community. Most of what the NIH in-house study is doing is available on the web so Dr Nath gave a short summary mentioning how the NIH is investing in this disease. ME/CFS is housed in the NINDS institute and considers ME/CFS as a neurological illness. The way that the NIH works is that there is an extramural budget (90%) which is there for people to apply for grant funding. NIH is unique in that it accepts grant applications from anyone, anywhere in the world. Then there is an intramural programme that involves a unique clinical research centre which consists of 70 different buildings on that campus. Three buildings that are joined together form a unit where all the clinical activity takes place. This is the only research hospital in the world where all patients attending come there only because they are taking part in some kind of research programme. Nobody can walk in just to be treated there. It is a gated place so one needs to have a permission to gain access to enter. Dr Nath sees patients in these buildings as well as has his lab there so it is a short distance from bench to bedside and back and forth thus aiding research. Patients can be admitted to this hospital as long as necessary. The study on ME/CFS is rigorously designed to concentrate on those patients that had a clear infectious onset. Once patients meet the criteria they are admitted a total of ten days and during that period of time an extensive battery of tests is being undertaken. They will then look at all the data that they have gathered to make sure they have not missed some kind of underlying disease which explains the patient’s symptoms. They also have a committee of five people who are experts in ME/CFS and they’ll go over the entire record of these patients to decide whether the patient truly meets all the criteria. After this the research team moves to phase 2 where patients are brought in again and this time patients are challenged by an exercise test and collect various kinds of parameters on them before and after. It is a very involved project and they aim is to recruit 40 patients and 40 controls. They anticipate that the study will take about four years to complete. They already have 13 patients and 16 controls recruited. There are a number of sub-studies also. Dr Nath said that even though the NIH is doing this study intra-murally they are happy to collaborate with anyone else. They also put a lot of effort in communication. There are monthly conference calls that they participate in. They have an open book policy and are happy to answer any questions. Dr Nath introduced Dr Brian Wallitt who is a rheumatologist and responsible for all the day to day activities of the study such as screening all the records, seeing the patients, making sure everything is co-ordinated and he has put together the team of people involved. The clinical team is critical in making sure everything works. Then there is a team of researchers who give their time to work on this project on top of their normal day to day duties.
Question from the audience to Dr Nath asking whether any additional ideas have come along since they started the testing of patients.
Answer: Dr Nath said that two things have been added
1/skin biopsy to look at the nerve fibres
2/muscle biopsy due to them finding that some people may have a disease that affects the muscles but looks like ME/CFS (looking at mitochondrial DNA as that looks different in the muscle than in the blood)
So for a variety of reasons they have started looking at the nerves and muscles.
Question was asked about the possibility of NIH speeding the process by employing researchers that would work on this project full time like the clinical team?
Answer: There is no barrier for the NIH to hire people and if they need people they’ll hire them. A lot of the samples will get processed at the end of the study to make sure all the samples are being processed using the same technology (the technology won’t be the same four years from now) instead of processing one sample at the time as they come in. Some samples are best sent out to commercial places for testing so those are decisions to be made as they go along.
Question How common are multiple infections (CMV, borreliosis, ehrlichia etc)?
Answer: What is required that the disease has been triggered by an infection. If people have subsequent infections they are not excluded but documentation of the initial infectious trigger is critical.
Question regarding vaccines and their role as triggers.
Answer: Dr Unger said the CDC take vaccines very seriously and she is an HPV expert in her other role and this is the first time these two things have merged. It takes large epidemiological studies to confirm links and so far they have not found any link in the US but they continue to look and monitor the situation. They are trying to gather data on paediatric ME/CFS and if they can get school wide surveillance then they’ll get the information needed.
Question Is adult ME/CFS seen as different from paediatric ME/CFS?
Answer: from Dr Unger. They see them as the same illness but recognise there are differences for example in that POTS is more prominent in paediatric cohorts. There is no way to distinguish these groups other than by age at this point. More data needed.
Question to Dr Unger about prevalence figures that are different (quite high) from the ones currently in use. Also the female to male ratio (42%) is different to the normally used ratios.
Answer: The presentation referred to the survey and the figure of 42% referred to % of responders to the survey being female.
Higher than normal prevalence figures reflect the fact that they were dealing with self- reported illness and that will end up in some false positives/false reporting but it is a way to start putting the picture together. Dr Unger said she linked this to the Canadian data which was the same kind of self-reported recording system where they found the same prevalence. This is a problem the public health is used to. They know they get a lot of unnecessary data (common colds) for example when they gather information on influenza but they can then compare this data to a smaller population from clinics.
Question to Dr Unger: Is there any plan to actually examine the patients to confirm the diagnosis or otherwise?
Answer: The study design and IRB is not to do follow ups on these patients. They try to get people to answer the phone and talk to them. Additional studies are needed to flesh out and understand the data.
Question to Dr Nath and Dr Unger on neuroinflammation. Have Drs Unger and Nath thought of reaching out to other areas of research such as HIV and cancer (HPV) as these areas have vast budgets and resources.
Answer: by Dr Nath: A lot of the knowledge gained from HIV is being applied to ME/CFS. All the immunology Dr Nath does and relates to neuroinflammation is gained from his HIV knowledge. The underlying biological systems are the same so knowledge gained from one disease can be applied to another. There is a lot of cross fertilisation.
Dr Whittemore said they have a representative from the National Cancer Institute in their trans NIH working group so they are actively involved and interested. The National Cancer Institute and the Institute of Aging have now funded four groups to develop new ways to measure fatigability which Dr Whittemore thinks is applicable in studying fatigue and PEM in ME once they develop their new methods.
Question on genetic studies in ME/CFS.
Answer: Dr Nath: Genetics is now the new fashion and everybody in any disease wants to find out the underlying genetic causes. It is not easy to figure that out because all of the dominant ones have already been discovered so you are looking at small effect sizes of multiple genes and those are harder to find and you really need very large sample sizes and proper controls. There is so much genetics going on that you’ll see a lot of data on ME/CFS that has been done or comes up but it will be harder to interprete.
Dr Whittemore said they are talking about international collaboration to get it done. She gave an example of epilepsy where they have collected 25,000 samples internationally to be sequenced in the US and that is the sort of level of numbers you need.
Quadram Institute Bioscience Update
Gut Microbiota in ME
Due to urgent business and sickness Professor Simon Carding and Shen-Yuan Hsieh (PhD student) were unable to attend so PhD students Katharine Seton and Fiona Newberry presented on behalf of them.
Katharine started by telling the Quadram Institute Bioscience (QIB) theory being that the intestinal viral infection alters the
gut microbes that can then lead to gut inflammation.
If there is inflammation this can lead to leaky gut.
If there is leaky gut the gut microbes can escape from the gut causing abnormal immune response to gut microbes ultimately leading to autoimmunity.
Katharine’s PhD project aims to look whether there is evidence of leaky gut - and to test this they are doing a
human study where they are recruiting severely ill ME patients from Norfolk and Suffolk ME/CFS clinic and the CFS clinic run by Dr Amolak Bansal in London.
It is a large area that they are covering so they have to travel quite far to collect the samples.
They are looking to recruit ten pairs of severe patients and household controls.
A household control is someone who is either related or not related to the patient but living with or caring for the patient.
It is important to use household controls because the environment has a massive impact on the gut microbes.
By using household controls they are hoping to identify disease related alterations.
Katharine’s experimental project involves collecting blood and stool samples, isolating immune cells and antibodies from the blood
samples and gut microbes from the stool samples.
Katharine is using numerous techniques to test if the immune cells react and bind to the gut microbes.
So far she has developed two techniques and found, based on the patients tested so far, that they have significantly higher levels of gut microbes that are
recognised by antibodies.
Fiona started by explaining She-Yuan’s (“Ernie”) work that involves isolating viruses from the stool samples.
It involves going through various steps of virus isolation (it is like a coffee filter) and at the end you get viral DNA that is put on a sequencer
and this tells what viruses are there and that is the main part of Ernie’s work.
The aim of this first part of the project is standardisation of the protocol for all of the patient samples.
The next part of the project is to find out what exactly are these viruses doing. Are they altering the microbiome?
The way he is doing this is by isolating specific viruses from the faeces and determining whether they kill the bacteria or not.
The ones that do have an effect on bacteria are then put in an animal model (mice) to test if the mice exhibit ME/CFS like symptoms after an exercise challenge.
Fiona’s own PhD project is to identify microbiome and virome alterations in severe ME/CFS patients.
All three PhD students are studying the same patients and the main question is what happens to the viruses isolated on the faeces.
This part of the project involves a lot of computer work and there are several problems involved in interpreting the results as
viruses are highly variable, only a small fraction has been identified and in a lot of the faecal samples it is impossible to know
what the viruses actually are and the tools used for analysis are massively underdeveloped. Fiona’s project involves developing a
programme that helps interpret the results.
Questions from the audience ranged from making the students aware of glyphosate and its possible effects on the gut microbiome, whether twins have been studied (not so far) and the usefulness of probiotics (the need to identify what is missing first before able to recommend anything).
Dr Peter Holger Johnsen
Double blinded, single center, placebo controlled, randomized clinical trial treating ME with FMT
Dr Johnsen first mentioned their recently published double blind placebo controlled faecal transplant trial (FMT) in irritable bowel syndrome patients (IBS). As they thought there are overlapping symptoms in ME and IBS they applied for a Norwegian research council grant to perform the first double blind placebo controlled trial of FMT in ME/CFS. Both diseases lack biomarkers and are disabling, the diagnosis is based on patients’ symptoms. In ME/CFS gastric problems are associated with abdominal pain and change in bowel habits.
FMT is transplantation of microbiota from a healthy donor to a patient’s gastrointestinal tract. FMT is an accepted treatment for C Difficile infection but in any other conditions it is considered experimental. The transplant can be delivered either to the lower or upper part of the gastrointestinal tract, normally through an endoscope but also using an enema. There are private clinics offering FMT (one in Florida and one in UK) and even websites with “Do it yourself” instructions. The Norwegian Health Directorate requires strict donor screening and FMT is considered in the same way as tissue donors. Enthusiasm needs to be balanced with caution regarding this treatment. FMT is used to target the immune system, metabolism, CNS and genes for antibiotic resistance. There are now about 200 clinical trials of FMT listed in the clinical trial registry. An example of an immune target was identified by a positive outcome in 3 out of four ulcerative colitis trials.
There is an overlap in IBS and CFS symptoms. Both have fatigue (50% of IBS patients find fatigue as a major symptom) and about 90% of ME/CFS patients have had IBS like symptoms at some point over the life time of their illness and 50 % have concurrent IBS.
There is bidirectional communication between the gut and the brain. The CNS can influence the microbiota by stress hormones and influence the gut epithelial barrier and modulate the immune response while the microbiota can influence the immune response to release anti- and pro-inflammatory factors that modulate the CNS. The microbiota can also trigger the release of neuroactive molecules. The cause and effect in ME/CFS is unknown. In IBS targeting the microbiota by changing the diet, taking pro- and prebiotics and FMT has been shown to be beneficial in relieving symptoms.
Dr Johnsen then went on to explain the results of their double blind placebo controlled study in IBS which showed 65 % improved in the active group vs 43% in the placebo group measured at three months after treatment. There was still improvement at 12 months but that improvement was not significant. They also measured the symptom of fatigue and at three months 60% in the active arm showed improvement in their fatigue scores compared to 36% in the placebo group. At twelve months the significant difference disappeared. Quality of life was 56% improved in the treatment group vs 32 in the placebo group after three months.
The IBS study led to the Comeback ME/CFS study with the hypothesis being that ME/CFS can result from the dysbiosis of the faecal microbiome and FMT can alleviate symptoms by restoring a healthy gut flora and cause symptom relief/remission of disease.
80 patients fulfilling Canadian criteria will be included and divided into active and placebo groups. Active group receives samples from healthy donors selected according to the European consensus guidelines and the placebo group receives their own processed stools. There will be a twelve month follow up with a primary endpoint at three months using the Chalder fatigue scale and a secondary endpoint at twelve months also measured using the Chalder fatigue scale. They will also do a neuropsychological test at baseline and at three months. As diet, probiotics and medication can influence the microbiota they will also do a food diary/medication use questionnaire. They will also obtain faeces, urine and blood samples at baseline and at three and twelve months to be stored in the biobank for later use with collaborators. They will collaborate with Simon Carding, QIB (metagenomics) and Maureen Hanson, Cornell University (biomarkers for disruption of gut epithelial barrier).
Questions: What is the reason for only transient disappearance of ME symptoms (personal experience).
Answer: Could be related to the gut virome. In a study involving ulcerative colitis patients those with lower viral loads responded best.
Question: Are patients stratified by those with IBS symptoms and those without.
Answer: Patients are stratified by age and gender and they’ll also use the De Paul Symptom questionnaire.
Question: Are parasites screened for?
Answer: Yes, as according to the guidelines.
Professor Karl Johan Tronstad
Cellular Energetics
Karl Johan Tronstad started by saying that the past two days had been very constructive and it is a really different atmosphere compared to normal scientific meetings.
His topic is cellular energetics and their approach to studies in ME/CFS.
Dr Tronstad works very closely with Drs Fluge and Mella and their translational research team at Haukeland University Hospital.
Samples are collected from patients attending the clinic, stored in a biobank and then the researchers try to find chemical changes in these samples that can be used in their laboratory experiments. Until now they have been working on metabolomics (metabolic profiling of the samples), some gene regulation and they also have a study where they try to identify ME in families by looking for gene variants that can be important for the disease.
They also use fibroblasts and targeted studies trying to find mechanisms and maybe biomarkers.
The team has been funded by the Kavli Trust, patients and their families and the Norwegian ME Association. Last year they received funding from the Norwegian Research Council and that project is trying to find out if an initial insult leads to defective energy metabolism.
The project has four goals
1/ Strengthening and extending the ME/CFS biobank
2/ Metabolic profiling of patient samples
3/ Identification of risk genes (based on the ME family studies using exome sequencing)
4/ Mechanisms and biomarkers that can be taken further
When you study a patient sample you get a snapshot of that point in time so one has to be careful of interpretation and to avoid this they do many different analyses. They are looking for changes in fuels that are circulating (sugars, carbohydrates, proteins that are degraded to amino acids and also lipids). They are also looking at specific factors that can be a source for an abnormal response.
In 2016, they published a paper that showed a change in the pattern of 20 amino acids and this change was linked to the central axis in energy metabolism. In a normal cell there are many back up pathways if one pathway is blocked so you may not see very much but the team thought that this change in amino acid pattern could mean something important. They are studying the meaning of this blockage and the cell’s ability to adapt to such a blockage. They also asked whether there is something in the patient’s blood that is causing the metabolic change. They took healthy, normal muscle cells and exposed them to sera from patients and healthy controls. The take home message was that there was a change in oxygen consumption (important for mitochondrial function) and also in lactate production. There is something in the patients’ sera that changes muscle cell metabolism but they do not know what it is and it can be quite complex.
They are now also using radioactivity labelling to try to see what is happening to the cellular fuels (not in the glycolysis but mitochondria). They label various substrates with radioactive markers and then measure CO2 coming out of the cells. They are not only looking at the nutrient flow but factors that may regulate this and to do this they try to learn from other conditions such as cancer, aging, neurodegeneration, diabetes etc. They try to do targeted approaches to find out which factors might be involved as these pathways can be affected by many things such as fasting, vigorous exercise, starvation and so on.
So far they have fibroblasts (skin cells) from one ME affected family and in this way can look out for mutations that may be the cause of the disease. They are measuring oxygen consumption of these fibroblasts under different nutrient conditions and they think they can see some differences in the cells’ ability to adapt to different conditions. These cells are not optimal cells to look at metabolic changes but they are cells that are easiest to obtain and can be stored in the laboratory for some time. Until now, they have worked with PBMCs that are easy to obtain but they cannot be maintained in the laboratory and fresh samples would be needed often to do such a study.
They also use some commercially available muscle cells.
There was a cartoon illustrating the team’s concept. The energy output needs to be balanced by fuel going in. This is being mediated by cell metabolism and kept quite constant in variable conditions. Cells cannot do more than their energy levels permit. Threats to this system can be such as reduced level of fuel, energy leak, metabolic obstruction, disturbed control and these may be overlapping and all may contribute.
The energy demand will also depend on different conditions (rest, work recovery). If there is a cellular obstruction as in the Tronstad team’s model then the cells need to use an alternative fuel source that may not be ideal.
This may lead to metabolic disruption and weakening of the system. The cells try to do damage control and maybe the system is not really resting. If you add increased energy requirements to such a system you may be overcharging the system and this is not sustainable. They are looking for a cellular marker for post exertional malaise.
They try to mimic and target these different conditions using laboratory cell models (Hela for example). They will investigate these mechanisms and target them with different kind of manipulations (pharmacological, nutritional and also genetic). They also aim to get samples from patients so that they can use a translational approach in the laboratory.
The way they can stress cells in a culture is to put them under nutrient deficient conditions, they can make restrictions for the total energy supply, they can control oxygen level but they can also use targeted methodologies to modulate specific metabolic programmes (pharmacologically or genetically) and they can also add specific inhibitors.
The conclusion is that there is suboptimal energy metabolism and that creates a weakness that may not be visible under every condition. They think these mechanisms are reversible and they are working on ways to rectify this.
Question Have the team looked at mitochondrial DNA in siblings of ME patients as mitochondria are inherited from the mother?
Answer If you are looking at mechanisms it is quite a complicated way to go as the mitochondria only code for 13 proteins that belong to the respiratory system. If there were a genetic defect you would see it in different means.
Answer by Maureen Hanson: They published a paper on mitochondrial DNA after sequencing 200 patients and 200 controls but they did not find any differences. They did find some differences that correlated with severity of certain symptoms but not having a disease or not.
Question: Any thoughts on mitochondrial supplementation?
Answer
It is difficult to come up with any recommendation. Based on the team’s review there is no reason for them to advice on anything regarding mitochondrial targeted treatment.
Professor Don Staines
Emerging TRP pathology: the way forward in pharmacotherapeutics and treatment
Don Staines talked about the emerging TRP pathology the NCNED is studying in Queensland, Australia. They are interested in a group of nonspecific ion channels called the TRPM3 ion channels. These are important in bringing in calcium into the cells. These are critical in several biochemical functions (mitochondrial, respiratory etc.) and the talk concentrated on TRPM3 expression in NK cells and the gastrointestinal tract.
There has been 30 years of research into NK cells in ME/CFS and the NCNED team use NK cells as the model but Dr Staines stated that what happens in NK cells probably happens in all the other cells that carry these ion channels as well. They have previously found reduction in NK cell lysis and this leads to immune dysfunction, impaired function of the NK cells. As they cannot access tissue in the brain and heart for example they use fresh blood samples instead. Frozen blood cannot be used for this research.
TRPM3 has more isoforms than any other TRP. One of the subtypes is non-functional and contaminates other TRP channels nearby.
When people say ME/CFS is a neurological disease one can say yes and no as all organ systems are likely to be affected by ME/CFS.
The NCNED group’s hypothesis is
1/ There is a significant link between TRP dysfunction and CFS/ME
2/ There is no relationship between TRP dysfunction and CFS/ME
Research question 1
They identified genetic difference in TRPM3 in CFS/ME compared to healthy controls and to understand these differences they need to examine TRPM3 expression on the cell surface
1/ Can they identify novel TRPM3 receptors on the surface of isolated NK cells from healthy controls?
2/ Is there a difference in TRPM3 expression between CFS/ME and healthy controls?
Next step is to examine what is the effect. Do calcium levels in isolated NK cells differ between patients and healthy controls?
In bright NK cells there is decreased expression of the ion channel, decreased transmission of calcium, changes in biochemistry and impaired lysis of the target cell.
Can the levels of calcium coming in and out of the cells be influenced pharmacologically? In vitro tests have been done using pregnenolone sulphate which increases the number of receptors but nothing else changes. Calcium levels are still low in the cytosol and endoplasmic reticulum. It made no difference.
They did additional tests by using drugs that block loss of calcium from the cells and this seemed to work. It demonstrated (in vitro) amenability to pharmacological intervention showing that ME/CFS is potentially reversible.
As TRPM3 receptors are located in the white matter of the CNS (brain and spinal cord), eye, trigeminal and ciliary ganglia, pancreas, gastrointestinal tract, cardiovascular system and is co-location with mACh receptors (e.g. lipid rafts) they may correlate with various symptoms ME/CFS patients’ experience.
Research question 2: Tissue Accessibility?
Until now, the work has been done in blood due to inaccessibility of tissue samples but they have now been able to get gut tissue. The TRPM3 expression is sparse in ME/CFS patients gut tissue compared to healthy controls.
Research question 3 involved muscarinic receptors. Can they identify and characterise them in the gastrointestinal tract of patients and healthy controls? Are there inflammatory changes in the gastrointestinal biopsies between ME/CFS and healthy controls?
mAChM3 is reduced in ME/CFS vs healthy control and IL-alpha is reduced in ME/CFS vs healthy control suggesting it is not the primary mediating pathology.
Conclusion: Impaired expression and function of TRPM3 ion channels affecting calcium signalling/stores suggests the primary pathology of ME/CFS.
Question:
Do you have a biomarker?
Answer (Don Staines):
This is always a difficult big/question to answer. The SNPs would be a beginning of a biomarker but there is a caveat that the results may be different in a different population.
Question:
What is the next stage?
Answer:
The damaged cells are amenable to pharmacological intervention and the task is now to start isolating various drugs and drug derivatives to look at.
Question:
Do you anticipate there being differences between cells from a single person so that there might be combination of chemicals that worked in some cells but might not work in others?
Answer:
Changes in the genes are different. We are all different. The test mentioned involved 20 to 30 patients. You take one person and their SNP profile may be different from the other person’s so you cannot say one drug fits all. What is tricky here is the concept of personalised medicine where you have to diagnose each case as it comes from a profile of SNPs and ion channels and there may be subtle differences in drugs and drug derivatives. Therefore, you may have to develop a cocktail approach to each patient.
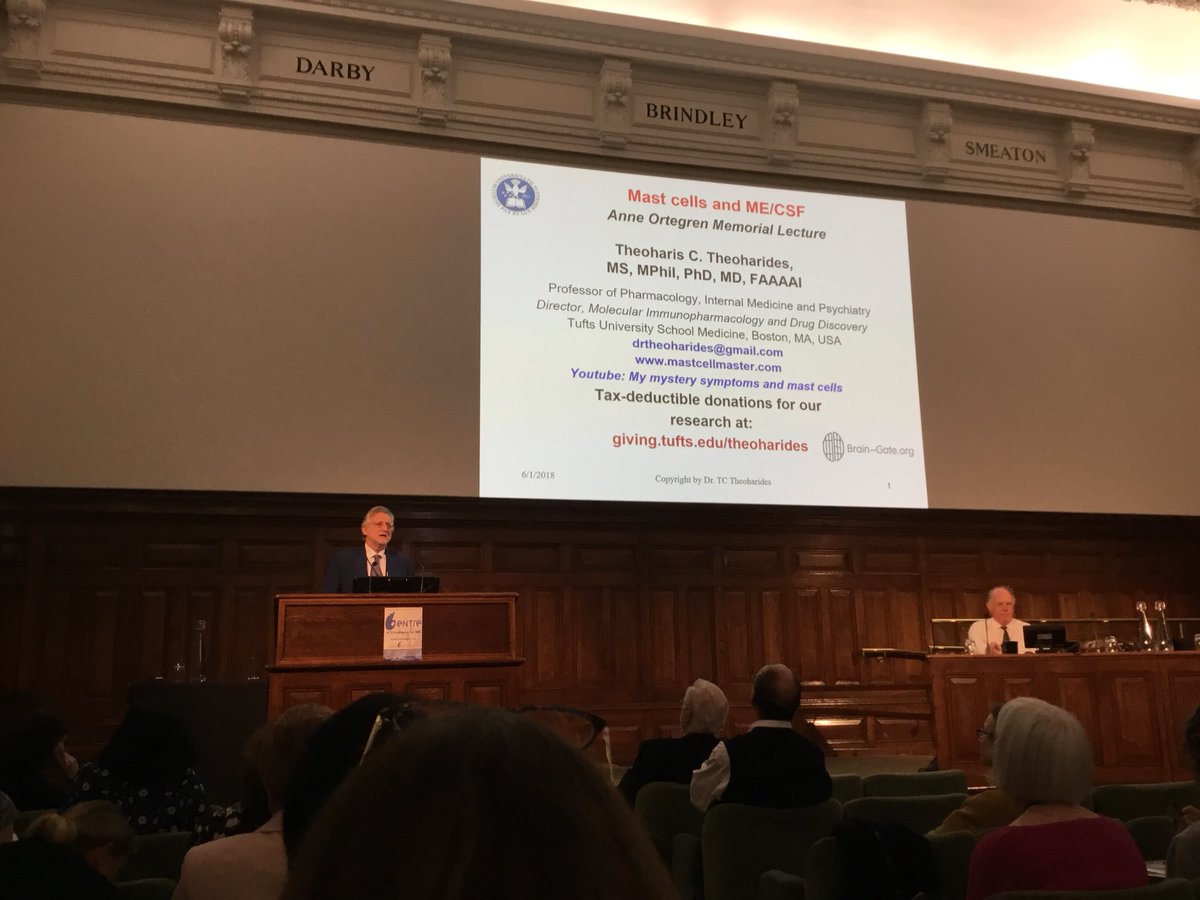
ANNE ÖRTEGREN MEMORIAL LECTURE - Professor Theoharis C. Theoharides
Mast Cells and ME

Remembering the influence of Anne Örtegren.
The lecture started with a tribute to Anne Örtegren.
Professor Jonas Blomberg opened the lecture by giving insight into the contact he had with Anne. It started five years ago.
Anne was like a good fairy guiding Professor Blomberg into the ME field.
Anne was very considerate, very knowledgeable and also a kind person. That was a very good introduction to ME research, patient advocacy and collaboration between researchers and patients which was new to Professor Blomberg.
He liked this collaborative approach. Within the Swedish and international networks emails were exchanged.
Anne was always helpful and sent good suggestions and found new research that the researchers should know about.
Then the emails that used to come rather frequently, stopped.
Later Professor Blomberg understood why.
Anne had intense and intractable pain and suffering.
It was understandable that she could not continue.
We should remember Anne as a very good proponent of the ME cause.
http://www.investinme .org/IIMEC13-news-180201.shtml
Professor Theoharis Theoharides
Everything Dr Theoharides was going to talk about could be found on his website www.mastcellmaster.com.
Mast cells are involved in allergic reactions and that is the tip of the iceberg. Why mast cells? Dr Theoharides referred to Anne’s symptoms of hyper reactivity and burning skin. Whether we call this “allergy” or “atopy” or “mast cell activation syndrome” we owe it to Anne to investigate the connection she described and find suitable treatments and a cure.
Atopy is caused by a zillion things and seems to attract ME and the more allergies and sensitivities one has the more likely the symptom severity is being affected or having the chance of developing the disease. There was a paper published recently to look at precursors for mast cells where they measured telltale signs on the surface of the precursors and they found more mast cell precursors in ME patients. Of course, they do not know where these cells go and what they do.
Mast cells are made in the bone marrow and travel via the blood but do not circulate. They home into tissues.
There are many different things that present as allergies such as angioneurotic edema, asthma, atopic dermatitis, food allergy, food intolerance, idiopathic urticaria and so on. All of these involve mast cells but only allergies are literally allergies yet mast cells not only participate in all these other diseases but are activated by other things other than allergies. Atopic diseases can be diagnosed using blood (IgE,IgG₄) but the most proper way is to collect 24h urine (kept cold) sample where they can measure breakdown molecules of two metabolites histamine and prostaglandin₂.
90% of patients that show up in clinic have shiny circles under their eyes and if you scratch the surface of their skin (under the arm or back for example) they get a red welt within a minute. This means the mast cells on their skin respond to pressure and not to allergens. This is a quick tell- tale clinical sign that might allow one to start thinking something is going on.
Many years ago, long before becoming involved in ME, Dr Theoharides and team started looking at other diseases and they showed that mast cells are involved in interstitial cystitis, fibromyalgia, autism but that does not mean that mast cells do exactly what they do in allergy. They can do a number of things depending on the trigger and circumstance. They can be triggered by numerous factors such as environmental factors, pathogens, peptides from the brain, growth factors etc. Mast cell looks like a soccer ball and it can explode and release its contents of which we mostly know histamine and then we use antihistamines to address the histamine after it has been released. We really need a good way of blocking this occurring.
What interested Dr Theoharides in this field that many patients with mastocytosis or mast cells that were super activated had cognitive problems, especially brain fog. Depending on what the mast cells release, they can affect every organ in the body, including the brain. Since the publication of this information in New England Journal of Medicine there has been a new insurance accepted diagnosis called mast cell activation syndrome.
There are two important factors. You do not need to have too many mast cells or allergies necessarily but the mast cells are activated by everything under the sun and the diagnosis includes neurological problems for the first time. All of these patients complain of brain fog as well as symptoms (flushing, headaches, hives, myalgias etc.) seen in ME patients.
Mast cells are not isolated. They talk to macrophages, T-cells and they have receptors on the surface that can be activated by bacteria, viruses, fungi, mold etc. They respond to heavy metals and herbicides.
Why do we think mast cells are involved in ME?
The hypothesis is based on the work on mast cells in the brain. If you take a cross section of blood vessels in the hypothalamus that regulate homeostasis in the body you can see red blood cells, endothelial cells, the pericytes that make up the blood brain barrier and the mast cells “hug” the blood brain barrier. Dr Theoharides and his team believe based on their work in autism that mast cells are involved in a look- a-like inflammatory response. Why hypothalamus? Because strangely it has as many mast cells per unit volume as one’s skin yet the brain does not get allergic reactions. So obviously these cells are doing something there and the more we can identify what they do the better for a number of diseases. We know that homeostasis is derailed in ME patients.
Many conditions worsen by stress, and we know that major stressors (mother’s stressors) during pregnancy makes the baby more prone to allergies. The more atopic conditions or tendencies the child has the more likely the child develops autism. This was tested in a mouse model where the mouse was stressed by being put into a confined space. Stress hormones called corticotropin releasing hormones (CRH) trigger the release of mast cells that open up the blood brain barrier. Together with neurotensin mast cells induce the dilation of blood vessels. When the blood brain barrier is opened up all kinds of toxins and potential pathogens get in whether from the environment or the gut.
Things get worse as when neurotensin sees the mast cells as it makes them grow receptors so they can respond to CRH and this becomes a self-amplifying process that cannot be stopped unless the mast cells are stopped. It may be useful to look at multiple triggers in combination rather than single triggers as smaller amounts of many triggers can do the damage. The team have measured biomarkers in Fibromyalgia and have shown that CRH and substance P were significantly increased in Fibromyalgia patients and they are known to stimulate mast cells to release chemokines. They are currently comparing ME patients to Fibromyalgia patients.
In summary so far:
Mast cells can explode in severe allergic reaction in which case histamine and tryptase are being released. A number of cytokines and pro inflammatory molecules are also being released without undergoing degranulation.
They also studied mitochondria and discovered that mitochondrial DNA together with CRH increases allergic responses. Mast cells are involved not only in allergic reactions but inflammation as well. All inflammation is not the same. Systemic sepsis is inflammation and it is called cytokine storm. If you have encephalomyelitis it tends to be generalised in the brain. If you have meningitis it is the lining of the brain and if it is in myelin that insulates the nerves it is Multiple Sclerosis (MS).
So what about ME?
Dr Theoharide’s take is that it is focal inflammation in the hypothalamic area and if we are talking about myalgic encephalomyelitis it should be myalgic encephalomyelitis in the hypothalamus and not necessarily the whole brain.
Dr Theoharides then talked about toxins that are in the environment ( seafood related toxins, spider bites, mold).
How to measure inflammation? Dr Theoharides measures both pro-inflammatory and anti- inflammatory marker molecules because the range gives more information than individual molecules alone.
How does inflammation occur in the brain?
It can be local or it can be materials coming in the blood and affecting the hypothalamus. The team’s hypothesis is that the mast cells activate microglia that are defenders of the brain. There are no white blood cells in the brain and if white blood cells get into the brain they
get recognised as foreign and get attacked and then you get MS. Microglia are like spiders with a web and neurons grow on the web and if microglia detect dangers they start to multiply and try to confine that area and get rid of it.
If something is coming from the periphery, how does it get to the brain?
Blood brain barrier might be disrupted and that is how it goes in but there is another way they can go in. There are tiny vesicles that are released from cells and they are called microvesicles or exosomes and it turns out they carry cargo to various places and they are so small that they get through the blood brain barrier. A study showing an increased number of microvesicles in the brain of autistic patients compared to healthy controls has been done and they are in the process of doing the same in ME.
They also wanted to know what happens to microglia if they are exposed to microvesicles.
They cultured human microglia in the laboratory and isolated microvesicles from an autistic patient and measured the main inflammatory cytokine IL1 beta. IL1 beta was raised but they did not know what the cargo was but thought whether it might be mitochondrial DNA so they measured mitochondrial DNA in the microvesicles and it was more than in controls.
Does it mean we have a biomarker?
It gives the team something to move forward with.
Danger signals in the pathogenesis of ME were listed as cachexins, electromagnetic waves, heavy metals, herbicides, inflammatory cytokines, mitochondrial DNA, mycotoxins, neuroendocrine disruptors, neuropeptides, reactive oxygen species, venoms and xenobiotics. The connectivity is unknown. Can they block it?
The team have been studying a class of molecules called flavonoids that are very good antioxidants and anti-inflammatories and they have shown that they block mast cells and microglia. Luteolin in particular was mentioned.
They had done a study on mice trying to induce fatigue by giving the mice poly (I:C) that mimics viral infection and then making the mice swim in cold water and they measured inflammatory molecules in the serum and in the brain after giving the mice normal chow or chow enriched with flavonoids.
The inflammatory molecules dropped down to zero when mice where given chow enriched with flavonoids.
In summary:
Mast cells talk to microglia. Microglia contribute to the symptoms of ME. For better or worse flavonoids could be used to treat brain related inflammation.
One needs to be sure other similar diseases are excluded.
They might be co morbid and some might be treatable. These are Chronic Inflammatory Response Syndrome (CIRS), Fibromyalgia Syndrome, Ehlers- Danlos Syndrome (EDS), Gulf War Syndrome, Interstitial Cystitis / Bladder Pain Syndrome (IC/BPS), Mast Cell Activation Syndrome (MCAS), Post-Lyme Syndrome and Post Traumatic Stress Disorder (PTSD).
Treatment Approaches- Exclude/Avoid
Exclude: Hypophysitis and pitutary adenoma, Mast Cell Activation Syndrome
Avoid: allergens, colourings, deodorants, perfumes, electromagnetic waves, flame retardants, heat, histamine rich foods (ripe avocados, ripe tomatoes, cheese, sardines, spices), plastics, preservatives and stress.
Treatment approaches: Brain Gain (a combination of supplements) for cognitive functioning, Caprylic Acid for mold exposure, antihistamines such as Cyproheptadine which increases appetite and is good for migraine prevention, Doxepin, Ibuprofen (anti-inflammatory), Propranolol (beta blocker).
Antacid is always added for stomach protection
Question: Would you measure tryptase?
Answer: Unless one has full blown mastocytosis tryptase is not elevated and it is not part of mastocytosis diagnosis. It is a good quick test and if it is negative then one can look for metabolitis in the urine.
Question: Do cannabidoids help with bone pain?
Answer: An audience member said they found CBD oil helped with pain. Dr Theoharides said he had no experience of it but it seems to work for epilepsy.
Word of caution for product quality in that FDA had found some CBD oil had been produced from plants that had been stored wrongly and been moldy so the oil contained toxins.
The same goes for all flavonoids and dietary supplements as the purity is not guaranteed.
Associate Professor Mady Hornig - Coulumbia University, New York, USA
Parsing heterogeneity in ME/CFS to accelerate discovery of tractable disease phenotypes
Mady Hornig’s presentation concentrated on trying to parse the heterogeneity of ME/CFS in terms of diagnosis and treatment.
Dr Hornig thinks of immune related brain disorders being based on the following three elements: genes, environment and timing and thinking even prenatally there could be some event that influences the person’s development over the course of their lifetime. Examples of disorders were given such as autism and ADHD in early life, MS and ME/CFS in middle life and Parkinson’s and Alzheimer’s in later life.
The programme at Columbia university relating to biomarker discovery has been wide from RNA based to protein based and DNA studies. They have tried to utilise all of these to make meaningful subsets.
Characteristics of the disease relate to length of illness, onset type, age at onset, disease severity, atypical features and comorbidities. Up to 70% of patients have comorbidities.
Allergy/Atopic disorder studies include asthma, seasonal rhinitis, atopic dermatitis, sinusitis, hives, eczema, hay fever and interstitial cystitis.
Neurological impairment studies involve excessive brain fog, perceptual impairment, attentional deficits and memory dysfunction.
Gastrointestinal dysfunction studies not only consist of microbiome but they are also looking into celiac disease, inflammatory bowel disease and irritable bowel syndrome.
Dr Hornig described the group’s previous immune marker studies into early disease versus late disease, where they described the immune exhaustion paradigm. These studies suggested there were meaningful subsets. She then went on to describe their more recent study on spinal fluid samples. They showed that there is a difference between patients with a classical presentation of the illness (viral onset) versus those with atypical based either over the course of the illness or presentation and who went on to develop other severe conditions later on such as cancer, MS or gulf war illness. IL7 and IL17 were low in the atypical group of patients. These patients have sparse inter-cytokine networks. The results were found before these individuals developed some of the other conditions mentioned and they fitted the ME/CFS diagnosis at onset.
We may think that classical ME/CFS involves increased microglial activation but based on this study the classical ME/CFS group had signs of less microglial activity.
They have also been thinking of allergic/atopic disorders as a subtype. What they found was increased pain and gastrointestinal disturbances and higher levels of endocrine disturbances were predictive of the allergic group.
They were also interested in severe cognitive dysfunction. There has been very little work done on cognitive sensory dysfunction. They’ll use cluster analysis to try to define cognitive dysfunction and ultimately see how this correlates with peripheral immune dysfunction and they hope to have spinal fluid samples from other cohorts to look at the central immune regulation.
They also looked at gastrointestinal dysfunction. The gut brain axis is going to be important in regulating normal health as well as disease. They used stool microbiome doing metagenomics and also predicted bacterial metabolomics in 50 cases and 50 controls. They then used topological data analysis to see how the data clustered together. They saw differences in patients with and without IBS in their metabolic profiles as well as their bacterial profiles. They saw particularly high levels of deethylatrazine (a herbicide common in ground water throughout the US) in all of the groups. It has endocrine disruptor effect. Vitamin B6 pathways were elevated in the non-IBS group. Patients were also grouped based on BMI.
They want to separate biomarkers which are stable versus fluctuate over time and which of them are disease associated versus state associated.
They are interested in the degradation of the herbicide deethylatrazine as a potent endocrine disruptor.
They have also done plasma metabolomics to see which metabolites may have come out of the gut or been transported by the short chain fatty acids into the blood stream of these patients. The cytokines and metabolites can affect the blood brain barrier.
Diet is very important as there some substances such as tryptophan that are important both in production of serotonin as well as downstream synthesis of melatonin which influences the circadian rhythm. Healthy CNS and immune function depend on balance.
Autoimmune disturbances may result from failed uptake of dietary antioxidant precursors in terminal ileum. Certain microbes may also lead to a more pro-inflammatory effect of Th17 and counter reduction of Treg cells.
They use deep data mining techniques in their biomarker discovery project. They want to look at both environmental exposures as well as genetic variants.
Question How does your allergy-testing correlate with standard allergy tests such as IgG and skin tests?
Answer Point taken. Patients’ self-reports were being used and objective measures have not been looked at yet except in that cytokines are allergy associated. Funding needed to do studies with proper measures.
Professor Maureen Hanson - Cornell University, New York, USA
Research at the Cornell Center for Enervating Neuroimmune Disease
 Maureen Hanson started by saying that there is a confounding factor in all the studies they do in that there is within group and between group heterogeneity. It is usually possible to control for age, gender, race, ethnicity, body mass index and length of illness but there are other factors that are very difficult to control for. These are things such as genetics (even identical twins have some differences in their genetics), initial trigger, co-infections, immunological history, current environmental exposures, activity level, symptom severity, medications and supplements and diet.
Maureen Hanson started by saying that there is a confounding factor in all the studies they do in that there is within group and between group heterogeneity. It is usually possible to control for age, gender, race, ethnicity, body mass index and length of illness but there are other factors that are very difficult to control for. These are things such as genetics (even identical twins have some differences in their genetics), initial trigger, co-infections, immunological history, current environmental exposures, activity level, symptom severity, medications and supplements and diet.
One way of dealing with this problem is to compare the same subject following provocation of symptoms or amelioration by treatment. This can give insight into disease pathology. Chances of studying patients in this way is to follow patients in the two treatment studies Cornell is collaborating with, the Norwegian FMT trial (Dr Peter Holger Johnsen) and an Ampligen trial (Dr Dan Peterson, Simmaron Research). They want to see if gastrointestinal barrier improves in the FMT trial and follow some blood biomarkers in the Ampligen trial.
Provocation studies also allow one to study patients that get worse and healthy controls who remain well. Then you compare to see what happens to the same person before and after provocation/treatment so they serve as their own controls and this reduces the need for controlling for several variables. You can also of course compare patients to healthy controls before and after provocation/treatment but having someone serve as their own control is going to be helpful in trying to figure out the illness. The way to make ME patients worse is to ask them to exercise so clearly exercise therapy is not something people should be doing since they are going to get worse. They do a two-day cardiopulmonary test and usually sedentary controls feel invigorated 24h after the test but if you are a patient you’ll have post exertional malaise and you will not be feeling good. The advantage of a maximal cardiopulmonary test is that you get a lot of physiological data (VO₂max, Oxygen pulse, Oxygen saturation etc.) A typical test only requires ten minutes of exertion compared to some submaximal tests that can last 30 minutes.
The collaborator in these tests is Dr Betsy Keller who has now tested 94 patients. Most of the patients came in to prove their disability and she has been able to group them into different subgroups depending whether it was their VO₂max, blood pressure or heart rate that went wrong to cause post exertional malaise. They are going to use this data to see if it correlates with several of the other parameters that they found changed in these patients even before they induced post exertional malaise.
Dr Hanson then talked about their NIH funded research centre. They have three research projects, administrative core, clinical core and integrative data analysis centre. They are recruiting ten patients and ten controls per year from each of the three clinical collaborating sites (Geoff More, John Chia and Susan Levine) making it 90 patients and 90 controls at the end of year three. The three research projects are oxidative stress and neuroinflammation (Dikoma Shungu), extracellular vesicles (EV) and signalling (Maureen Hanson) and single cell expression ( Andrew Grimson).
Dr Shungu’s group has already shown that there is increased lactate and reduced glutathione in the brain.
Why would you have increased lactate in the brain?
One possibility is mitochondrial dysfunction that is causing the energy metabolism to dysfunction leading to increased anaerobic glycolysis and lactate is the product of the anaerobic glycolysis.
Why is there mitochondrial dysfunction?
This is unknown but possible causes could be infection and immune dysfunction. Whatever is happening is causing oxidative stress and if glutathione is lower it means one cannot mitigate oxidative stress. So for some unknown reason toxic free radicals are being created causing oxidative stress.
What happens when you have oxidative stress?
They cause chemicals called isoprostane formation in phospholipids and this results in membrane degrading enzyme. When the membranes are attacked by this enzyme you have isoprostane release in the blood stream. This has been documented in an ME/CFS paper and what isoprostanes do is cause constriction of blood vessels and that means reduced blood flow. There is good evidence from many papers that blood flow is reduced in the brain in ME/CFS. Reduced blood flow causes hypoxia and hypoxia can cause increased glycolysis due to reduced oxygen leading to elevated lactate. Hypoxia can also cause mitochondrial dysfunction and the mitochondria themselves can cause oxidative stress and release oxygen radicals. This all leads to a vicious cycle and there is a need to find out what causes the vicious cycle in the first place.
To do this work Dr Shungu is going to do MRI and PET scans before and 24 hours after an exercise test. This involves 30 patients and 30 controls.
A Japanese study found evidence of microglial activation in ME/CFS. Microglia are immune cells in the brain and they have mitochondria that have a protein called TSPO on the outer membrane. TSPO is a known marker for neuroinflammation in many diseases (MS, brain injury). To measure the amount of TSPO one uses a radioactive probe that binds to this protein and then you measure the amount of radiation to see if there is microglial activation. This is what was done in the Japanese study. The higher the amount of the probe the worse cognitive dysfunction and a higher amount of the probe also correlated with higher amount of pain. Dr Shungu is going to replicate the Japanese study.
The second project is led by Dr Hanson and this involves drawing blood before and after two exercise tests. This blood is going to be used for a number of different assays looking at metabolites, extracellular vesicles (size and amount), vesicle protein cargo and RNA sequencing. There are many collaborators doing these experiments. The group has results of some interesting metabolite studies and are hoping to publish those soon.
Dr Hanson went on to explain extracellular vesicles. There are three kinds. There are exosomes, microvesicles and apoptotic bodies. Extracellular vesicles are present all over the body, they carry nucleic acids such as RNAs, they carry different functional proteins on surface and as cargo, are used in communication between cells and they can regulate immune response. Extra cellular vesicles cross the blood brain barrier and may be involved in neuroinflammation.
Brain cells themselves can also give out extracellular vesicles. These cells gives researchers easy access to study the brain.
Dr Hanson’s group has done a pilot study in size and number of extracellular vesicles in plasma of 35 patients and 35 controls. The patients’ physical function scores (SF-36) are lower than those of controls and when they looked at the extracellular vesicles they found that exosomes were increased in patients at baseline.
They are going to do RNA sequencing to see how miRNA cargo differs between EVs in plasma of patients and controls. The vesicles contain miRNAs and miRNAs are particularly potent regulators of gene expression.
They can both up and down regulate genes and therefore effect the cell function. They are also going to do protein profiling of EVs.
The third project by Andrew Grimson is going to look at gene expression in single cells before and after exercise. As this is a very expensive method they are going to analyse gene expression in single cells before the first and before the second exercise test when post exertional malaise has already been induced. That should give a good idea what is going on.
There have been many reports of immune system abnormalities in ME/CFS and that is why Dr Hanson believes calling this an enervating immune system disease is suitable and this really is a neuroimmune disease.
One problem though is that the findings are inconsistent. There are 46 publications where people have analysed RNAs in immune cells and these have just not given a consistent story so we do not have a major conclusion that comes out of these many studies.
One problem may be that the previous studies have studied all of the blood cells together or all of the lymphocytes together. There are many immune cells and by studying all of them together something important may be missed. By analysing single cells previously missed findings may be found.
Last thing needed to do is to see if there are correlations between the data to give insights into new mechanisms.
The goal of the Cornell group is to identify biomarkers for specific diagnosis of ME/CFS and also to develop biomarkers for treatment that do not need to be specific. Biomarkers help understand pathophysiology of ME/CFS and may reveal existing drugs that could be used to treat the disease or help develop new drugs.
Question: Could one of the bad actors be an endogenous retrovirus that is being expressed and causing problems?
Answer: There is at least one study that was unable to find an expression of endogenous retroviruses. However, like many things in this illness there needs to be replication and expansion with the latest methods so hopefully someone takes this further. There will be some information regarding endogenous retroviruses in the single cell studies. There are also other groups that are doing RNA sequencing of immune cells.
Professor Markku Partinen - University of Helsinki, Finland
ME/CFS from a sleep medicine perspective
Markku Partinen started by confirming the WHO classification of ME being neurological. He said unfortunately from his experience as a neurologist it does not guarantee that neurologists will see ME patients. He said his hypothesis was similar to the ones presented by Mady Hornig and Theoharis Theoharides.
He explained disease being made up of factors such as genome that explains 25% and 75% being explained by ambiome and microbiome. Ambiome is the environment and everything contained in it.
Sleep is necessary for life. 100% of rats die within a month if they are not allowed to sleep. Billions of dollars have been spent on the exercise industry but exercise is not vital for life whereas nutrition and sleep are.
He then explained the orexin system that is the most important system for sleep. It is in the hypothalamus regulated by the central circadian clock. Last year the Nobel price was given to three researchers who demonstrated that each cell in the human body has a peripheral clock. This system is also connected to the autonomic nervous system, the endocrine system, emotional regulation and energy balance. Sleep is described by a flip-flop theory. After a time awake sleep follows and in sleep disorders there is no flip-flop between these two states but the balance is broken.
Orexin cells are glucose sensing cells.
When glucose is down orexin cells become activated resulting in more alertness. When glucose level goes up orexin goes down and one becomes sleepy. When ME patients eat carbohydrates they feel worse. A high carbohydrate meal makes one sleepy and fatigued. If ME patients are at the limit of hypoglycaemia, almost acidic, they usually feel better.
Orexin cells are also salt sensing cells.
When salt goes up orexin goes up and this leads to wakefulness and increased blood pressure.
When salt goes down orexin goes down leading to sleepiness and lowered blood pressure. ME patients often lack salt which causes low blood pressure and increased heart rate.
Position, immobilisation syndrome.
There are a lot of studies of ME and exercise but very few studies on position. Experience from studies in the elderly shows that exercise is not important but position is. If a person is horizontal for a long time salt goes down and these patients will develop hyponatremia.
Just by elevating the top half of the bed a little leads to sodium going up. This is something that should be investigated in ME patients in a controlled way.
It is a vicious cycle for ME patients that cannot remain upright leading to salt going down.
Why is sleep necessary?
Sleep is necessary for the energy of the brain and brain clearance. It also has a role in immune function and memory function. The amount of sleep needed is individual (between 6 and 9 hours) any time between 9pm and 9am.
“Astrocyte-Neuron-Lactate-Shuttle”.
Glucose penetrates the blood brain barrier. Most of it will go to the astrocytes to be stored as glycogen. Another place for stored glycogen is the liver. By glycolysis lactate is formed. When a person is awake neurons use lactate as fuel. Some of the previous talks discussed evidence of increased lactate in the brain of ME/CFS patients and also increased lactate when measured in the periphery.
Dr Partinen stated that it is normal that lactate is accumulated in the astrocytes during deep sleep and this is very good and essential for good neurological function when people are awake. Another important function is the glutamate –glutamine cycle. Without working glutamate cycle the lactate shuttle is not working. If people are not active in the daytime they are not producing energy in the night time.
Clearance of metabolites.
In the deep slow wave sleep the brain’s interstitial fluid is increased by more than 60%. Glymphatic (glial-lymphatic) flow helps clear accumulated substances in the deep slow wave sleep phase. Possible reasons for unrefreshing sleep are behaviourally induced insufficient sleep, medications (bentzodiazepenes), mental hyperactivity and circadian rhythm disorder. Sleep disorders must be ruled out before giving a patient an ME/CFS diagnosis but sleep disorders may sometimes be co-morbid.
Autonomic nervous system
There are two parts, the sympathetic and the parasympathetic system. The sympato-vagal balance regulates the immunological homeostasis. If, theoretically, there is a very low vagal tone (low parasympathetic tone) the risk for inflammation increases. On the contrary if the vagal system is stimulated tolerance is increased.
In a simplistic way by lowering the parasympathetic tone immunity decreases and inflammation increases. To improve vagal tone needs to be increased by vagal stimulation or the sympathetic load needs to be lowered by increasing fitness to a sufficient level but not too fit. PEM after exercise in ME is partly due to this system. Important things are relaxation and good sleep and sometimes beta blockers can be used.
Sympathicotonia
Many ME patients are sympathicotonic which means that their sympathetic tone is dominant. This is a good thing and many top athletes are like this.
They perform well under pressure but get emotional when pressure is off. Many ME patients have been sporty or mentally very active so they belong to this group and then something happens and they become unwell.
In sleep studies blood pressure can be measured at every heartbeat. During normal sleep blood pressure goes down and vagal tone increases to induce relaxation. In insomnia there is no lowering of blood pressure and during the whole night the system is sympathicotonic.
This is exactly the same way that dogs sleep. They sleep but they are constantly alert to any noises around them. They are never in a deep slow wave sleep. ME patients and insomniacs do not go into deep slow wave sleep and this leads to the lymphatic system not working and there is no good energy formation. There have not been many polysomnographic (PSG) studies in ME but the few studies that have been done show that subjective sleep quality is poor but there are no significant measurements in cortical differences.
Partinen’s group decided to measure the autonomic tone in their PSG sleep study. In normal healthy people parasympathetic tone increases but their study showed that the parasympathetic tone in ME patients decreased. They do not know the reason why this happens but there is clearly something wrong with the autonomic control relative to sleep. In this small study ME patients were compared to tired controls but when they compare ME patients to normal healthy controls the difference is much higher (study underway).
The team’s hypothesis is that ME patients have abnormal deep N3 -sleep. Parasympathetic tone is decreasing instead of increasing. This leads to dysfunctioning of the glymphatic system and lack of brain energy.
In 1934 there was a publication by Lapage that used the term “Autophilia” and Dr Partinen theorises based on this paper that due to reasons such as genetics, microbiome, pregnancy, infancy some people develop autophilia.
These are the persons that develop autopathias (allergies, atopy etc.), spasmophilia, neurological symptoms and psychiatric symptoms (e.g., anxiety is a problem in the autonomic nervous system). In ME one can find all these symptoms. In childhood these patients tend to be sensitive, flushing easily, experience fainting, travel sickness and nosebleeds. They are often lean and catabolic and have lower resistance to infections. As adults they are emotional, sensitive, excitable, mentally active, creative, culturally active and sporty.
In conclusion: There is abnormal N3-sleep that causes lack of brain energy and problems with glymphatic flow. Autophilia is a predisposing factor and restoring sleep will help in regaining homeostasis. Avoid medications but use sleep hygiene, CBTi (insomnia CBT), nutrition and perhaps H1 antagonists in very small doses (e.g., doxepin) and also vagal stimulation (no studies on this yet).
Question What are your thoughts on “owl” patients whose sleep is reversed?
Answer It is a complex problem because normally people should sleep when it is dark and be awake when it is light. There are some patients who feel better if they keep their reversed sleep pattern. Whatever we look at (hormones or white blood cells) there are circadian rhythms and they vary. There are no studies asking whether patients feel better at a certain time of the day and what is their worst time of the day.
Question You mentioned vagal stimulation. There are suggestions such as gargling or singing very loudly can help vagal stimulation. The person asking the question found singing loudly improved their sleep.
Answer That is possible and vagal stimulation is now used in intractable epilepsy and they may even put electrodes inside the brain but there are now some external stimulators as well. Studies should be done to test this properly.
Question There is a saying: “Time spent sleeping is never time wasted” mainly because sleeping is healing. Are forceful sleep hygiene measures good for patients?
Answer Theoretically the best time to sleep is somewhere between 10pm to 9-10am. If one can choose then it is better to go to sleep earlier and wake up earlier.
The important thing is to have at least 6h of sleep. Interestingly they have followed Parkinson’s disease patients over several years and their hypothesis was that if these patients had less sleep there would have higher mortality but the result was the opposite.
Patients who slept less than 6h had lower mortality.
They looked at all kinds of variables and found that patients that were optimistic despite their many problems had better outcomes. ME is a serious disease but the mortality is not very high. Is it so that despite severe symptoms there is still internal hope.
Question The more exercise I do during the day the longer I sleep and then I am more likely to feel more ill the next day, with bad headaches. There is a paradox in that sleeping more makes one feel worse. Conclusion is to sleep less and do less exercise to avoid increased headaches.
Answer This is a touchy area because theoretically if you do a lot of exercise you sleep well until you overdo it and develop overtraining syndrome. In ME one important thing is the position when sleeping. Elevation of the head is important. If you sleep too long mental function gets worse and that is why sleep deprivation is used as treatment in serious depression. Sleeping too much is worse than sleeping too little. The hours needed to sleep vary individually.
Professor James Baraniuk - Professor of Medicine, Georgetown University Medical Centre, USA
James Baraniuk presented his “Year End” report. They have an exercise model that they have used for ten years. They do an extensive set of questionnaires (about 50) and these are done online so that the patient can stop any time they want to and carry on later. The physical and history part is now 50 pages long and it can take up to four days to complete. It is not something a GP can do in eight minutes.
Dr Baraniuk is trying to work with the common data elements to try to develop the key questions that should be asked in every study so that the patient populations from all around the world can be standardised.
They also do allergy skin testing and the rate of positivity is the same in ME/CFS as in the control group. They have now done this in their fourth cohort. The levels of antibodies to allergy IgE are also equivalent between the two groups. Dr Baraniuk does not believe there is an increase in true allergic disease but there is an increase in sensitivity.
After talking to the participants they do an MRI and this includes an MRI during the cognitive test so that they can see if there are differences in the regions of the brain that are activated while the participants are doing the memory test. After this participants do an exercise test that is similar to the one described by Dr Hanson except that Dr Baraniuk’s participants do a submaximal test (at 70% of the person’s predicted maximum heart rate) which lasts 30 minutes as opposed to 10-12 minutes as described by Dr Hanson.
The participants can increase their heart rate up to 85% of their predicted maximum that is the same as cardiac stress test. They do not have to do 30mins. If they want to stop earlier they can stop and that would essentially be the person’s maximum.
Dr Baraniuk finds that his research participants’ day one and day two tests are highly reproducible.
After the second day exercise the participants do their second MRI to see if there are areas of the brain that have changed while they do their thinking and are those changes caused by the exercise and whether this is a model for exertional exhaustion. Finally, everyone who is agreeable gets a lumbar puncture. These participants are kept overnight to reduce the risk of spinal headaches.
The talk then went into discussing hypotheses including depression, pain and tenderness, exercise, postural tachycardia which is not the same as POTS, orthostatic intolerance, MRIs and some results from the CSF studies.
Depression
The depression scale used is a Center for Epidemiological Studies- Depression (CESD) questionnaire involving 20 questions with a scale of 0 to 3. The maximum score is 60 and if one’s score is 16/60 or more one is classed as depressed. This has been shown in 28 studies involving over 22,000 people. The problem is the scale has a 30% false positive rate.
One can do a factor analysis as the questionnaire can be broken down to four factors that are grouped together from the 20 items such as somatic, depressed, anhedonia (lack of pleasure) and interpersonal. The somatic factors are fatigue, sleep, cognition, effort, bother, talking less and appetite change. These four factors have been known for decades but nobody has ever bothered to score them in any patient population.
Dr Baraniuk’s group did this and discovered that using this scale 24% of the US population is at risk of depression and 54% of ME/CFS patients are at risk of depression but this score is biased as it is caused by high somatic domain scores (sleep, cognition etc.). It is the same thing for Gulf War Illness. Depression in ME/CFS discounted based on this evidence.
Pain
Pain is not in the SEID criteria because it does not differentiate CFS from other diseases such as Fibromyalgia. Dr Baraniuk says he has a big problem with how these diseases are defined and to bypass that he wanted to know about tenderness. Does 4kg pressure hurt?
The Baraniuk team uses a spring-loaded gauge to measure pain and the person being measured is in charge during the procedure. They use this on all of the 18 fibromyalgia pressure points and they can then calculate a score for average pain. The score for healthy people is about 7kg of pressure. The CFS group peaks at 4kg. The same thing happens when patients breath in formaldehyde or any other chemical, are exposed to bright lights or loud sounds.
The threshold is broken. An ambient background noise can become a loud and overblown when you have CFS. It is not imaginary but a very real broken switch. It is a hypothesis.
Submaximal exercise
When they did this they were expecting to see similar results to those of the VO2max stress tests. They did not see any difference in day one and day two results. They were identical and overlapped.
The test is up to 30 minutes but people can stop earlier. If people can only do 2 minutes on the first day they can only do 2 minutes on day two as well so it is highly reproducible and turns out to be useful as far as the MRIs are concerned. It also means that if there is a decrease in VO2 in the maximal test there is something magical happening after the Baraniuk participants stop.
We need to know how many people in the VO2max test actually have decreased performance, how much is that decrease and we need to know the sensitivity and specificity particularly if this is going to be used as diagnostic for CFS and certainly if it is being used for disability purposes.
Result: No difference in performance between day one and day two submaximal exercise tests.
Postural tachycardia
In previous research on Gulf War Illness (presented at IiME by Rakib Rayhan) they found 1/3rd of patients developed POTS after day 1 of submaximal exercise. Lying down they would have their normal heart rate and before exercise after they stood up from lying down position their heart rate would increase by about 12 beats.
After exercise 1/3rd would have an increase of at least 30 beats when they stood up and this is a definition used for POTS. This was an unexpected result. They got funding for a verification study in GWI that has now been finished but has been rejected for publication and that is what happens for verification studies.
They found that the START (Stress Test Activated Reversible Tachycardia) group had brain stem atrophy and this is similar to what Richard Kwiatek (Australia) reported in CFS. They then did the same study in their CFS group and report similar findings to GWI START group.
Dr Baraniuk encouraged all exercise study groups to do lying to standing heart rate measurements before and after exercise to disprove his findings.
To find out which groups had POTS they took dizziness scores lying down after exercise and all three (CFS with no heart rate change, CFS START and CFS POTS ) groups had similar scores. After standing up all three groups had again similar scores and this made
Dr Baraniuk think what orthostatic intolerance really is. Is it a difference in sensitivity coming from the vestibular system that one is feeling dizzy and light headed even when lying down and it has nothing to do with one’s heart rate or autonomic system.
Result: Exercise does not worsen orthostatic intolerance.
MRI
There are some changes but it is not that big. They can conclude that those groups that have changes in their heart rate have worse brain function after exercise.
Cerebrospinal fluid & biomarkers
miRNA levels were higher in people who did not exercise and they went down after exercise.
It is not a robust enough diagnostic marker for CFS but it has led to some ideas about what might be going wrong. If the miRNA level goes down one has more messenger RNA and one can make more protein and that protein will have more function. It looks like exercise in CFS leads to increase in some particular enzymes such as Insulin Llike Growth Factor 1 receptor, Transforming Growth Factor Beta Receptor 1 which are very important for proliferation of brain cells.
They have also looked at where these are found and they are in the microglia and choroid plexus which is a vascular region where most of the cerebral spinal fluid is being created. This gives some hints as to where dysfunction might be found after exercise challenge.
Conclusion: CFS is not depression, CFS is somatic, tenderness is increased, there is cardiac effect, MRI effect and CSF changes.
Question The effects of activity may not be visible the day after exercise/activity but later on.
Answer One thing the Baraniuk group is looking at is how much exercise is needed to cause a delay in the response. A curious thing is that sometimes a small effort leads to an immediate collapse and a bigger effect may have a longer delay.
Question A patient with POTS went to get tilt table testing and managed to get their doctor to insert a Hickman line. They now start the day with a litre of saline and that has improved the patient’s POTS. Does anyone else have the same experience? It seems a drastic measure.
Answer It is drastic. Dr Baraniuk said he has had one patient that had a central line and would infuse two litres and then go shopping and come back and do another two litres and go to sleep and they felt good. Also the patients that get saline after their spinal tap brighten up.
Dr Baraniuk recommends Gatorade to his patients as it is impossible to get insurance companies to pay for saline infusions.
Professor Ron Davis
Revolutionizing biomedical research through technology development
Ron Davis talked about the Stanford group’s latest discoveries and future plans. All their work has been supported so far by the Open Medicine Foundation (OMF).
They have a scientific advisory board and many of them were in attendance at the colloquium and conference (Maureen Hanson, Jonas Bergquist, Øystein Fluge, Ron Tompkins and Wenzhong Xiao). OMF have just funded Drs Tompkins and Xiao to set up clinical research at Harvard University.
One thing that has been clear to Davis’s team for some time is that they need an assay for a biomarker as so many patients (including Dr Davis’s son) have been told that there is nothing wrong with them because all routine tests come back normal. Dr Davis’s son is now severely ill. He cannot talk or read and Dr Davis still takes blood samples from him regularly and they run the same tests on him as doctors do and he is perfectly normal. The problem is that the routine tests are no good.
The focus of the team is now to prove that the patients are not healthy and they are being compared to healthy controls to see if there is a clear difference. That is task number one.
The next task is to find out if they can distinguish ME/CFS from another disease. This is very difficult to do as for one thing one needs to do all the other diseases.
Dr Davis is not sure this is necessary. What is necessary is to work with physicians to discuss with them what they need to know for a diagnostic test of this type or can they diagnose patients using some other criteria, by just talking to the patient.
Seahorse Instrument
The Stanford group has done some standard testing using the Seahorse instrument. They get best results by using isolated T-cells from patients and stimulating those cells and then measuring the energy production. The results have been reproducible.
If they do not stimulate the T-cells the results are more variable and it is also dependent on the time the patients have last eaten.
It is difficult for the patient not to be allowed to eat before they come in for testing. This test is also very expensive.
Nanoneedle
Another tool the Stanford group has developed is the so-called Nanoneedle. This tool measures electrical impedance that is a very sensitive electrical measurement. They make 400 measurements/second. Once they have finished taking a sample they have made 1 billion measurements. This is much more useful than medical devices that make just one measurement.
The Nanoneedle can be made commercially and if made in large numbers they will not be expensive. The Stanford group could make them for $1 to $5. They have now also figured out how to clean them so they do not have to remake them.
The measurement is done using a blood sample with red blood cells removed and then only a drop of blood is needed. A healthy person’s measurement looks flat on a graph and it is the same for CFS.
They reasoned that CFS patients’ cells need to be challenged so they added sodium chloride salt to make the cells work harder and then their impedance increases compared to the healthy controls. This same test can be used to see which antibiotic works on cultured bacteria and it can also be used on tumours. Physiological change will change the impedance. It is a cheap way of doing testing and the results can be obtained real-time. This might be useful as a diagnostic tool.
The team has also used the Nanoneedle to test how drugs work on the cells and they have found a number of drugs that seem to be able to get rid of this impedance effect. It is unknown if these drugs turn out to be useful or not.
Dr Davis showed an example of one of their experiments to show there was a very big difference between patients and controls, something that has only 1 in 10 million probability of occurring by chance.
They have done a few experiments to understand what works in this assay and this is called “The Plasma Swap Experiment”. The initial thought was that it is in the cell so they tested that doing a plasma swap. They took plasma from CFS patients and put it on healthy cells and vice versa.
They find that the signal they get tracks with the plasma and not the cell. That even suggests that the cells are healthy but there is something in the plasma that is causing this effect.
They do not know what it is yet but it is something that needs to be figured out as it is going through the entire body and may be causing some of the effects. If they can figure out what it is and what size it is they can try to figure out how to remove it and that could be treatment.
Microfluidic Device
Another device that the team have tested is a microfluidic device and they are collaborating with Professor Anand Ramasubramanian on this. This device measures the deformability of red blood cells. The idea is that red cells have to go through a device that is a bit larger than a lot of the capillaries in the human body.
If cells are not deformable they get stuck when they go in and when they reform they go slower through the device. The amount of elongation of the cell can be measured also. This is easy to do. The device needs refinement to make it smaller but they do see difference already in that the red cell entry is slower, transit velocity is slower and the elongation capacity is less in ME/CFS.
This does not currently work as a diagnostic tool as there is a lot of variance. This is an inexpensive and simple test. They will use Atomic Force Microscopy to measure deformability accurately.
Biomarker-Free Sorting
Another device the Stanford team has come up is a Biomarker-Free Sorting of Rare Cells from Blood.
It is a device that measures magnetic levitation. This means that they can suspend something in magnetic fluid if they put a magnet on it. This allows cells to be suspended very quickly.
Blood is put in the device and when the magnet is put on the cells will quickly go into density in a long tube. This device was developed for cancer to separate tumour cells from the white blood cells. The device can separate lots of different cells. Each run on this device costs only 5 cents. CFS patient’s results on white blood cells showed variation and density and some of the results were near normal and it turns out the patient had bacterial infection at the time of better results. The bacterial infection made the patient feel better not antibiotics. There are other patients who report similar saying fever makes them feel better.
Dr Davis thinks it is the bacterial infection that makes them feel better not the fever. In general the patients’ cells are light.
The team want to look at what happens in bacterial infection to make patients feel better.
Portable, mobile health platforms that use smartphones as computers allow rapid sample preparation, blood cell separation and count.
Biomarker Bake Off
Next task is going to be a biomarker Bake Off. This means all the samples coming in are being run on all these devices (nanoneedle, microfluidic blood flow, magnetic levitation, Seahorse and metabolomics).
Robert Naviaux found some metabolomic markers so they are comparing their findings to his finding. This will give five different instruments to look at the consistency. The reason for doing this is that there might be some exceptions and things do not work quite right but the other diagnostic tool did work right and is measuring something different. So in fact one might need to use two different instruments. They do not want many false negatives.
They also need to look at other diseases and how well the tests perform in those. That is when they need the help of physicians because it is possible that other diseases will show the same behaviour. The biggest goal is to show that the patients clearly are not healthy.
A Big Data Approach to Understanding ME/CFS
This project is funded by OMF. It involves 20 very severely ill patients. The project cost about $2million. The patients are bedbound or at least house bound and could not attend clinics.
They have also done a study of 15 families where there is more than one affected family member including unaffected members. It is unfortunately not uncommon to have more than one family member affected. There is a reasonable chance that there is something genetic going on in these families. The data is not yet available.
Hypothesis
Most people think that the way to do research is that you create a hypothesis and then you do a test to try to rule out that hypothesis. That is actually wrong according to Dr Davis. He says NIH has got it wrong. That is not a scientific method but that is what the NIH requires if you write a grant proposal. The scientific method is observation and then hypothesis.
Without observations random hypotheses are being formed based on nothing and we will never get there. What you want is an observation and that observation leads to an idea and that is the hypothesis. You are testing the hypothesis based on something that has been observed. That is how all science is done.
Why they say that when you write a grant you test a hypothesis and inevitably you do new observations and that is the basis of the next experiment and that can keep going on and on. What happens when you start a new disease? You have to make observations and then you can generate hypotheses.
Dr Nath’s talk showed that this is exactly what he is doing. He is making lots and lots of observations. There is no hypothesis there. So the idea is to create as much data as they can and that is what they are doing and that is why it is taking so long to even talk about it. It is a massive undertaking to analyse the data.
Findings so far
They have found that CFS is negatively correlated with depression. They also tested cell free DNA for traces of viruses that patients tell they have or had when they first became ill. Even if the organism is not in the blood their DNA will be.
They tested multiple regions of the viruses using a multiplex assay. The result was there were no viral infections that were different from healthy controls or that the healthy controls had more viruses that ME/CFS patients.
Dr Davis said that the result makes him suspect that patients have something else that feels like a viral infection. Inflammation for example can make people feel as if they had a viral infection. Most of the viruses they tested for do not do anything by themselves.
It is the body itself that does the signalling to tell that there is something wrong. The reason Dr Davis was stressing this point was to tell that if patients do not have a viral infection they should not be taking antivirals.
It is not healthy. The reason being that antivirals generally target the synthesis of the DNA from the virus and it works because they are very primitive DNA preliminaries. They can be inhibited without inhibiting the human preliminaries but the problem is that mitochondrial preliminaries are primitive also and some of the antivirals can inhibit mitochondrial preliminaries.
Given the fact that there is some evidence of lack of mitochondrial activity in ME/CFS it is probably not a good thing to take antivirals. Dr Davis thinks patients should not take anything they do not need.
New Probing
Dr Davis and his team are also doing new probing as they have found that ME/CFS patients’ gene expression is similar to the expression from trypanosome (Sleeping sickness). The symptoms for Sleeping sickness resemble those of ME/CFS. One notable symptom is sleep reversal and that is common in ME/CFS too. This discovery led to the decision to develop multiple DNA probes against all known trypanosomes and parasites.
The West African trypanosome is very easy to detect in the blood but the East African one is very difficult to find. They also hope to make probes against RNA viruses that is not easy as RNA is not stable in the blood. This approach would allow them to look at a lot of infecting organisms. There are a lot of possibilities and maybe it is a new virus involved in ME/CFS and there was the excitement with XMRV. They have done a new microbe discovery project once and that came out empty.
Heavy Metals
Some patients have told Dr Davis they have heavy metal contamination and they need to detox from the heavy metals. The team have done urine analysis of all the severely ill patients and have found that they do not have heavy metals. However, they found that these patients are low in essential metals.
They have a hypothesis of this. One is that patients are low in essential metals as they are detoxing and removing essential metals. The way the urine tests were done did not detect mercury so the team took some new patients to test this by doing a hair analysis.
They found that high mercury is associated with low selenium (antioxidant) and the patients that had higher mercury levels had got it through eating a lot of fish. A little bit of a surprise was a patient from Finland who had a fair amount of uranium which is probably environmental and they do not know the medical consequences of this.
Gene Expression
The gene expression study in the severely ill patients showed a lot of changes in gene expression in the immune system and that means there is a lot of immunology going on and the team are not surprised by that. These same patients have high cytokines as well.
The team also want to look at the autoimmune system and what they are looking for is T-cell activation. They are now adding single cell analysis to this project. T-cells eliminate cells that are infected with any pathogen. If the T-cells find something foreign in the body they amplify and this is called T-cell expansion.
They have found T-cell expansion in ME/CFS and that means T-cells are recognising something. Dr Davis’s team have looked for a foreign agent but have not found anything. The T-cells could also be seeing self and that would be an autoimmune disease.
It could also be something else that is triggering the immune system and then it would not be an autoimmune disease.
Whole Genome Sequencing
Dr Davis’s team have also done whole genome sequencing. There are some genes that are different. Some of them are involved in NK-cell recognition. They are now going to do HLA and KIR sequencing. They continue to explore DNAH11, FAM20C, KIRs and NRXN1 (neurexin, a very large gene expressed in the brain).
They also have found a lot of metabolic changes and you see a lot when you look at different small molecules in the blood. They see activation of the immune system, a lot of genetic and metabolic changes. They have also done the microbiome.
Future Work
Looking at metabolic traps (combining metabolite and genomic data taking a systems biology approach). The idea is that due to genetics and inflammation that gets started the pathways are not working as they should due to mutations. If this is true it is probably easy to fix according to Dr Davis. This has not been tried before. It should be inexpensive and should only take a few days to get the patient out of this “metabolic trap”. This research is not aimed at getting a publication out but trying to figure out what it is. Dr Davis wants everyone to start thinking this way to help find a solution. Dr Davis is optimistic.
Question: There have been a number of reports that cholesterol is high in many ME patients even though they are non- obese. Cholesterol could change in the discourse of the blood due to temperature (from 37 to 34 degrees) changes. Could that change affect the impedance measurements in your instrument?
Answer: The disease affects a lot of lipids, metabolism and that is why the white cells are light and that is why a lot of the metabolites are lipid containing. They do not know why this is but one thing they see is a fair amount of mutations in fat metabolism in the patients compared to healthy controls. If one cannot metabolise fats they accumulate and then you get feedback systems and it affects all sorts of other fats as well. You ought to get rid of them so you may not be able to oxidise them in the mitochondria and you may have to oxidise them in ER.
Question continued: What might be a good control group that would mimic ME patients. Perhaps a group of people with high cholesterol levels?
Answer: People with high cholesterol would probably be genetically determined and it is probably very narrow in terms of the lipid problems they have. It also looks like a lot of the glucose is shifted into the sorbitol pathway which then goes to fructose and then to fatty acid synthesis so your body is even making fat. There is no understanding of this at the moment but there is something that is off in the lipids in the patients.
Question relating to improvement under fever conditions that has been also observed in autism (speaking during fever but not otherwise) and the other question relating to red cell deformability. In sickle cells there are certain processes that are oxygen dependent and some that are not. Do you or can you control oxygen sensing in your system?
Answer: There is a close relationship to autism. The metabolites look very similar. There is obviously a difference in onset time. Bob Naviaux has treated some autistic children with Suramin that blocks the purinergic receptor and he got a great deal of improvement. Dr Davis has been trying to get hold of Suramin but he cannot. However, a new manufacturing plant is being set up in the US and it may be available by the end of the year. The nice thing is that Suramin is not very toxic and curiously, it is also used for trypanosomes.
Question: Have you got plans of trialling any of the drugs tested on the impedance device on patients?
Answer: We are trying drugs that are FDA approved but as we are not physicians we cannot so we partner with other physicians and that would be something we are going to discuss with Ron Tompkins. We found one drug that seems to improve the ATP production and that is a drug called Adavan. It helps but only for a few hours and it is used for crisis management only.
There was a general question related to what was needed most to make progress. Dr Davis said money to pay for staff salaries for at least two years ahead. There is a lot of head hunting going on and if people do not know about their future salaries for longer than 6 months ahead they move on.
The conference concluded with comments from Dr Ian Gibson .
Conference Presentations from IIMEC13
BRMEC8 - International Research Colloquium, London 2018

Invest in ME Research organised and hosted the Biomedical Research into ME Colloquium number 8 in May 2018.
Ninety researchers from fourteen countries attended the two-day meeting.
The collaborative atmosphere and resulting collaborations from the Colloquium will help further progress research and ultimately help patients.
Use this link to go to the BRMEC Colloquium page.
IIMEC13 Pre-Conference Dinner Presentation
Carol HeadLos Angeles, USA
Carol Head, President of the USA organisation Solve ME/CFS Initiative (SMCI), will be giving the pre-conference dinner lecture.
Carol has worked at the Los Angeles Times in a variety of marketing and strategy roles; she served as associate vice president of the 1984 Los Angeles Olympic Organizing Committee; she has been active in community affairs with an emphasis on human rights for women and girls and amelioration of extreme poverty, serving on three national nonprofit boards, including service as a board chair.
Carol is also a founder of Project Redwood, a venture philanthropy fund that supports creative approaches to alleviating extreme global poverty. She received a Bachelor of Arts in English from Wellesley College, and earned an MBA from Stanford University.
Solve ME/CFS have, in recent years,established the Ramsay Award Program which provides awards for research teams around the world.
Amongst the successful recipients of the Ramsay grants are research groups which are performing research funded by Invest in ME Research - and this has enabled the research funded by the charity to be extended.
Carol will be discussing on SMCI’s research and advocacy programs and looking at the recent changes in the landscape of ME/CFS in the United States.
Opening of 13th International ME Conference - IIMEC13
Dr Ian Gibson#InvestinMEresearch
Former Dean of Biological Sciences, UEA
Dr Ian Gibson was the former Labour MP for Norwich North. Dr Gibson worked at University of East Anglia for 32 years,
became Dean of the School of Biological Sciences at UEA in 1991
and was head of a cancer research team and set up the Francesca Gunn Leukaemia Laboratory at UEA.
In 2011 Dr Gibson received an honorary doctorate of civil law from UEA.
A scientist, politician and academic - Dr.Ian Gibson was uniquely qualified to comment on how science and politics have become intertwined.
Other Links
-
References
ME Research Update at Centres for Disease Control, USA
Dr Elizabeth R. UngerChief of Chronic Viral Diseases Branch, National Center for Emerging and Zoonotic Infectious Diseases, Centers for Disease Control and Prevention
Elizabeth (Beth) Unger, PhD, MD, received an undergraduate degree in Chemistry at Lebanon Valley College, Annville, PA. She then earned her PhD and MD in the Division of Biologic Sciences at the University of Chicago where she also began a residency in pathology. Her residency and fellowship was completed at Pennsylvania State University Medical Center. During this time, Dr. Unger developed a practical method of colorimetic in situ hybridization. This work led to interest in tissue localization of HPV and ultimately to her initial appointment to CDC in 1997 to pursue molecular pathology of HPV and CFS.
Dr. Unger has served as the Acting Chief of CVDB since January 2010 and has 13 years of experience in CVDB, where she has participated in the design and implementation of CFS research and HPV laboratory diagnostics. During this time, she was co-author on 25 peer-reviewed manuscripts related to CFS, including the often-cited descriptions of the Wichita and Georgia population-based studies. In addition, Dr. Unger has been instrumental in efforts by WHO to establish an HPV LabNet and serves as lead of a WHO HPV Global Reference Laboratory. She is co-author of 142 peer-reviewed publications and 24 book chapters and serves on the editorial board of six scientific journals. In 2008, for her HPV research accomplishments, she received the Health and Human Services (HHS) Career Achievement Award.
Dr Unger has been selected to serve as the Chief of the Chronic Viral Diseases Branch (CVDB) in the Division of High-Consequence Pathogens and Pathology (DHCPP), National Center for Emerging and Zoonotic Infectious Diseases (NCEZID), Centers for Disease Control and Prevention (CDC).
-
References
NIH Common Data Elements
Dr Vicky WhittemoreProgram Director in the National Institute of Neurological Disorders and Stroke at the National Institutes of Health in the United States.
Dr. Whittemore is a Program Director in the Synapses, Channels and Neural Circuits Cluster. Her interest is in understanding the underlying mechanisms of the epilepsies including the study of genetic and animal models of the epilepsies.
The major goal is to identify effective treatments for the epilepsies and to develop preventions. Dr. Whittemore received a Ph.D. in anatomy from the University of Minnesota, followed by post-doctoral work at the University of California, Irvine, and a Fogarty Fellowship at the Karolinska Institute in Stockholm, Sweden.
She was on the faculty of the University of Miami School of Medicine in The Miami Project to Cure Paralysis prior to working with several non-profit organizations including the Tuberous Sclerosis Alliance, Genetic Alliance, Citizens United for Research in Epilepsy (CURE), and the National Coalition for Health Professional Education in Genetics (NCHPEG).
She also completed a four-year term on the National Advisory Neurological Disorders and Stroke Council.
Dr. Whittemore oversees a grant portfolio that includes basic, translational and clinical studies on epilepsy. These include grants on sudden unexpected death in epilepsy (SUDEP), the genetic epilepsies, and seizure localization studies. In addition, she oversees a grant portfolio on myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and fatigue. Her additional interests are in research on global health issues, stigma, and co-morbidities.
-
References
Challenges in study design and identification of patients with post-infectious ME
Dr Avindra NathNIH National Institute of Neurological Disorders, Bethesda, Maryland, USA
Dr. Nath received his MD degree from Christian Medical College in India in 1981 and completed a residency in Neurology from University of Texas Health Science Center in Houston, followed by a fellowship in Multiple Sclerosis and Neurovirology at the same institution and then a fellowship in Neuro-AIDS at NINDS.
He held faculty positions at the University of Manitoba (1990-97) and the University of Kentucky (1997-02).
In 2002, he joined Johns Hopkins University as Professor of Neurology and Director of the Division of Neuroimmunology and Neurological Infections.
He joined NIH in 2011 as the Clinical Director of NINDS, the Director of the Translational Neuroscience Center and Chief of the Section of Infections of the Nervous System.
His research focuses on understanding the pathophysiology of retroviral infections of the nervous system and the development of new diagnostic and therapeutic approaches for these diseases.
Links
.-
References
ME Research Developments at Quadram Institute
Katharine Seton and Fiona NewberryPhD Students, Quadram Institute Bioscience, Norwich Research Park, UK
The Quadram Institute is an interdisciplinary institute maximising the unique cluster of academic excellence and clinical expertise at the Norwich Research Park, working alongside the food and pharmaceutical industries
.
-
References
ME Research Developments at Quadram Institute
Dr Peter Holger JohnsenUniversity Hospital of North Norway, Harstad, Norway - Internal Medicine
Dr Johnsen works in the medical department at the University of Northern Norway in Harstad.
He is currently involved in the clinical trial of FMT which is being funded by the Norwegian Health Council. Five million Norwegian kroner has been awarded for the trial.
The study is supported by Norwegian Research Council. Together, it will be included 78 participants who either receive treatment with FMT from a healthy donor or placebo.
The study is double blinded, which means that neither participants nor scientists will know who received the treatment from donor or placebo before the study ends.
Startup with the inclusion of participants begins during Summer 2018.
Links
.-
References
Cellular Energetics in ME/CFS
Professor Karl Johan TronstadProfessor Institute for Biomedicine , Tronstad Lab, Bergen, Norway
Professor Tronstad completed his graduate studies in biochemistry at the University of Bergen (UiB) in 2002. As postdoc at the Haukeland University Hospital, he studied bioactive compounds with the potential to modulate mitochondrial functions in cancer cells. In 2005 he was recruited to the Department of Biomedicine, UiB, where he started his research group to investigate metabolism and mitochondrial physiology. His laboratory seeks to better our understanding of how defective mitochondrial homeostasis may disturb cell physiology, and how this may be involved in mechanisms of cancer and Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS).
Karl was involved with the recent paper to come from Bergen - Journal of Clinical Investigation Insight.
The Tronstad Lab investigates cell metabolism and mitochondrial biology and we are very fortunate that he can spare time to participate in the Colloquium.
Specialisms:
Metabolism, Cell biology, Mitochondria, Biochemistry
-
References
Emerging TRP pathology: the way forward in pharmacotherapeutics and treatment
Professor Don StainesThe National Centre for Neuroimmunology and Emerging Diseases (NCNED), Griffiths University, Australia
Professor Staines has been a public health physician at Gold Coast Population Health Unit.
He has worked in health services management and public health practice in Australia and overseas.
His interests include collaborative health initiatives with other countries as well as cross-disciplinary initiatives within health. Communicable diseases as well as post infectious fatigue syndromes are his main research interests.
A keen supporter of the Griffith University Medical School, he enjoys teaching and other opportunities to promote awareness of public health in the medical curriculum. He is now Co-Director at The National Centre for Neuroimmunology and Emerging Diseases (NCNED), Griffiths University in Australia
ANNE ÖRTEGREN MEMORIAL LECTURE - Mast Cells and ME
Professor Theoharis TheoharidesTufts University, Boston, USA
Professor of Pharmacology and Internal Medicine, Tufts University, Boston, USA
Theoharis Theoharides is Professor of Pharmacology and Internal Medicine, as well as Director of Molecular Immunopharmacology and
Drug Discovery, in the Department of Immunology at Tufts University School of Medicine, Boston, MA.
He was born in Thessaloniki, Greece, and graduated with Honors from Anatolia College.
He received all his degrees with Honors from Yale University, and was awarded the Dean’s Research Award and the Winternitz Prize
in Pathology.
He trained in internal medicine at New England Medical Center, which awarded him the Oliver Smith Award “recognizing excellence, compassion and service.” He also received a Certificate in Global Leadership from the Tufts Fletcher School of Law and Diplomacy and a Fellowship at the Harvard Kennedy School of Government. He has been serving as the Clinical Pharmacologist of the Massachusetts Drug Formulary Commission continuously since 1986. In Greece, he has served on the Supreme Advisory Health Councils of the Ministries of Health and of Social Welfare, as well as on the Board of Directors of the Institute of Pharmaceutical Research and Technology, and he is a member of the International Advisory Committee for the University of Cyprus School of Medicine. He first showed that mast cells, known for causing allergic reactions, are critical for inflammation, especially in the brain, and are involved in a number of inflammatory conditions that worsen by stress such as allergies, asthma, chronic fatigue syndrome, eczema, fibromyalgia, migraines, mastocytosis, multiple sclerosis, psoriasis, and most recently autism spectrum disorder.
He has also shown that corticotropin-releasing hormone (CRH), neurotensin and substance P, peptides secreted under stress, act together, and with the cytokine IL-33, to trigger mast cells and microglia to secrete inflammatory molecules. These processes are inhibited by the novel flavonoids, luteolin and tetramethoxyluteolin that he has helped formulate in unique dietary supplements and a skin lotion. He has published over 400 scientific papers (JBC, JACI, JPET, NEJM, Nature, PNAS, Science) and 3 textbooks with 29,887 citations (h-factor 84) and he is in the top 5% of authors most cited in pharmacological and immunological journals. He has received 37 patents and trademarks, including three patents covering the use of luteolin in brain inflammation and autism: US 8,268,365 (09/18/12); US 9,050,275 (06/09/15); US 9,176,146 (11/03/15).
Acting as Advisor, he was instrumental in the development of ibuprofen (Upjohn), Cetirizine (UCB) and Niaspan (Kos). He is also the Scientific Director of Algonot, LLC, as well as President of Theta Biomedical Consulting and Development Co., Inc., of BiomedAdvice, LLC, and of the nonprofit Brain-Gain.org. He is a member of 15 academies and scientific societies. He was inducted into the Alpha Omega Alpha National Medical Honor Society and the Rare Diseases Hall of Fame. At Tufts, he served on the Curriculum, Students Promotion, Grievance, Faculty Promotion and Tenure, as well as Strategic Planning Committees. He received the Tufts Excellence in Teaching ten times, the Tufts Distinguished Faculty Recognition Award twice, the Tufts Alumni Award for Faculty Excellence, Boston Mayor’s Community Award, and the Dr. George Papanicolau Award, as well as Honorary Doctor of Medicine from Athens University and Honorary Doctor of Sciences from Hellenic-American University. He is “Archon” of the Ecumenical Patriarchate of Constantinople.
Links
Associate Professor Mady Hornig
Associate Professor of Epidemiology, Columbia University Mailman School of Public Health
Mady Hornig, MA, MD did her undergraduate studies as a College Scholar at Cornell, received an MA in Psychology from The New School for Social Research and an MD from The Medical College of Pennsylvania and completed her residency in psychiatry at The Medical Center Hospital of Vermont and an NIMH/NRSA Neuropsychopharmacology Fellowship at the University of Pennsylvania. Her research leverages large epidemiologic cohorts, novel bench science and animal model studies to determine how microbial, immune and toxic exposures impact upon the brain across the life course, resulting in disorders such as autism, attention-deficit/hyperactivity disorder (ADHD), Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal infection (PANDAS), mood disorders, schizophrenia, myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and age-related cognitive deficits.
Dr. Hornig is internationally known for her work in the growing research arena exploring the mechanisms of gut-immune-brain axis functioning, seeking clues to both the understanding of the roots of dysfunction as well as uncovering pathways that strengthen individual resiliency. She has a keen interest in how diet, exercise and environmental factors affect each individual’s intestinal bacteria – the so-called gut microbiome – which then influences brain function through alterations in blood-borne molecules.
She has identified naturally-occurring substances that appear to strengthen resistance to certain disease states affecting the brain, and is pursuing these as candidates for prevention and intervention in ME/CFS and autism. She uses immune profiling, metabolomic, proteomic, epigenetic and microbiome approaches to identify prenatal and birth biomarkers for brain disorders in large prospective studies in Scandinavia as well as the US. She is also applying these approaches to uncover markers of disturbed immunity and metabolism correlating with the severe clinical deficits that underlie ME/CFS, work launched with support from the Hutchins Family Foundation/Chronic Fatigue Initiative, the National Institutes of Health and the crowd-funding initiative, The Microbe Discovery Project. Perhaps most exciting is that new ME/CFS subsets that appear to have different triggers and may respond differentially to treatment are now being identified through her work.
Dr. Hornig’s approach is enriched by her unusual combination of decades of experience as a clinical researcher, her acumen in defining novel neuropharmacological and nutritional approaches for brain disorders and her ability to carefully tease out factors that enhance resiliency to disease.
In 2004, Dr. Hornig presented to the Institute of Medicine Immunization Safety Review Committee and testified twice before congressional subcommittees regarding the role of infections and toxins in autism pathogenesis and has lectured on ME/CFS throughout the world. She has over 120 peer-reviewed publications, has edited several books, and has received many academic awards. Her work has been featured by the New York Times, the Los Angeles Times, The Washington Post, The Wall Street Journal, The Atlantic, Discover Magazine, Nature Medicine, Science, Wired, the Huffington Post, O Magazine, CBS News, and This Week in Virology.
-
References
Research at the Cornell Center for Enervating Neuroimmune Disease
Professor Maureen HansonLiberty Hyde Bailey Professor, Department of Molecular Biology and Genetics, Cornell University, New York, USA
Department of Molecular Biology and Genetics, Cornell
Maureen Hanson is Liberty Hyde Bailey Professor in the Department of Molecular Biology and Genetics at Cornell University in Ithaca, NY.
Previously she was on the faculty of the Department of Biology at the University of Virginia in Charlottesville and an NIH NRSA postdoctoral fellow at
Harvard, where she also completed her Ph.D. degree.
While most of her prior research has concerned cell and molecular biology in plant cells, she began a research program on ME/CFS after noting at a
2007 IACFS meeting the paucity of molecular biologists studying the illness.
Her lab was part of the 2012 multicenter study organized by Ian Lipkin's group at Columbia University to assess the actual role of XMRV in ME/CFS.
ME/CFS from a sleep medicine perspective
Professor Markku PartinenProfessor of Medicine, University of Helsinki, Finland
Professor Partinen is a neurologist and an internationally well-known opinion leader and expert in sleep research and sleep medicine.
He is currently working as Research Director of the Helsinki Sleep Clinic, Vitalmed Research Centre.
He works also at Haartman Institute, University of Helsinki, and at Akademiska Sjukhuset, University of Uppsala.
His expertise covers sleeping, nutrition (what to eat), and other aspects of modern life and well-being.
His current research projects include narcolepsy, Parkinson's disease, insomnia, traffic accidents and daytime sleepiness.
He has published more than 250 articles in peer-reviewed international journals, several books and chapters.
He was recently (Now 2015) elected as the new President of the Finnish Parkinson Association. Professor Partinen is also a member of the European ME Research Group (EMERG) and European ME Clinicians Council (EMECC).
-
References
"Year End" Report
Professor James BaraniukProfessor of Medicine, Georgetown University Medical Centre, USA
Professor of Medicine at Georgetown University Medical Centre, washington, USA
James N. Baraniuk was born in Alberta, Canada, south of Banff. He earned his honours degree in chemistry and microbiology, medical degree, and
unique bachelor's degree in medicine (cardiology) at the University of Manitoba, Winnipeg, Canada.
Thereafter, he moved to Akron, OH, USA, for his internship and internal medicine residency at St Thomas Hospital.
After another year of internal medicine residency at Duke University Medical Center, Durham, NC, he trained with Dr C.E. Buckley, III, in allergy and clinical immunology. He moved to the laboratory of Dr Michael Kaliner at the National Institute of Allergy and Infectious Diseases, Bethesda, MD, and there began his long-standing collaboration with Dr Kimihiro Ohkubo.
After 2 years studying neuropeptides, he joined Dr Peter Barnes' laboratory at the National Heart and Lung Institute, Brompton Hospital, London, UK. Dr Baraniuk returned to Washington, DC, and Georgetown University, where he is currently Associate Professor with Tenure in the Department of Medicine.
-
References
Professor Ronald Davis
Professor of Biochemistry and Genetics at the Stanford School of Medicine in Stanford, California, USA
Ronald W. Davis, Ph.D., is a Professor of Biochemistry and Genetics at the Stanford School of Medicine in Stanford, California.
He is a world leader in the development of biotechnology, especially the development of recombinant DNA and genomic methodologies and their application to biological systems.
At Stanford University, where he is Director of the Stanford Genome Technology Center, Dr. Davis focuses on the interface of nano-fabricated solid state devices and biological systems.
He and his research team also develop novel technologies for the genetic, genomic, and molecular analysis of a wide range of model organisms as well as humans.
The team's focus on practical application of these technologies is setting the standard for clinical genomics.
.-
References
Plenary Session



 The mainstreaming this field of research has been one of the major achievements of the BRMEC* Colloquums and the IIMEC* conferences.
The mainstreaming this field of research has been one of the major achievements of the BRMEC* Colloquums and the IIMEC* conferences.